Itchy, red, watery eyes that won’t quit? If you’ve ever rubbed your eyes until they burned, only to feel worse afterward, you’re not alone. Nearly 40% of people in the U.S. deal with eye allergies every year, and it’s getting worse. With pollen counts rising due to climate change, more people than ever are waking up to swollen eyelids and eyes that feel like they’ve been rubbed with sandpaper. This isn’t just a nuisance-it’s a daily battle that affects sleep, focus, and even your mood.
What’s Really Going On in Your Eyes?
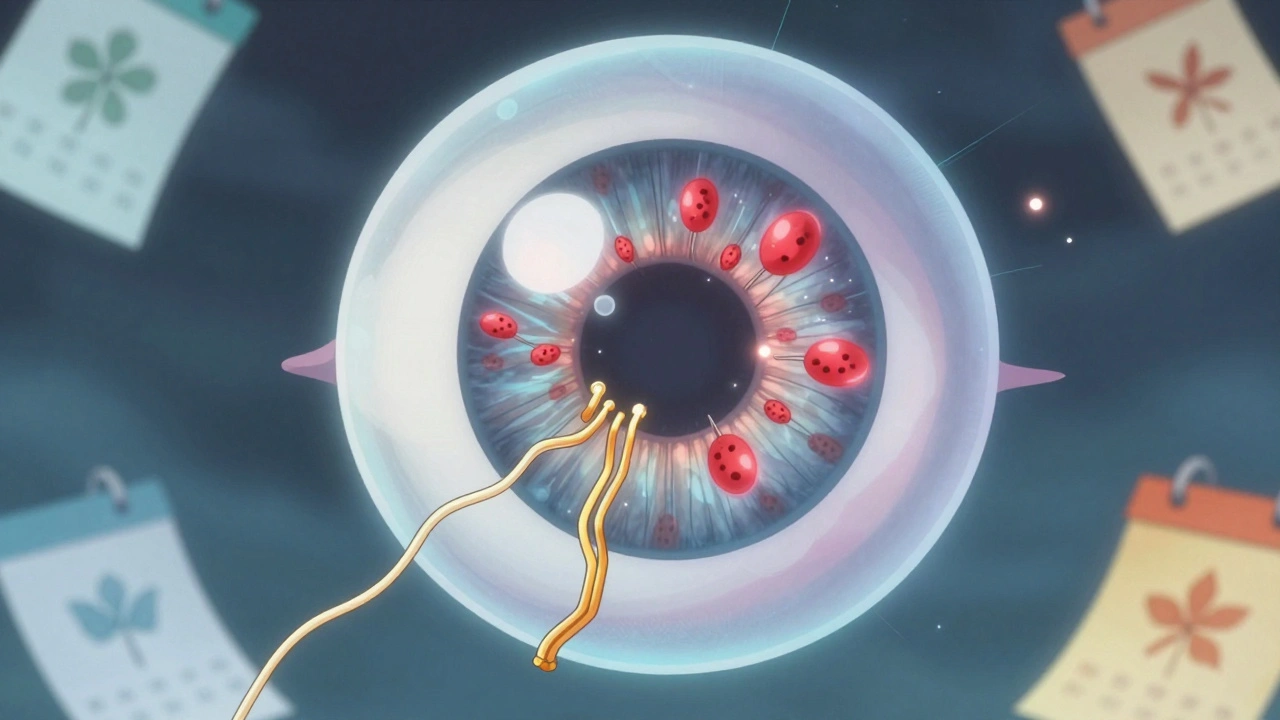
Eye allergies, or allergic conjunctivitis, happen when your eyes react to things in the air-pollen, mold, dust mites, or pet dander. These allergens don’t cause infection. Instead, they trigger your immune system to overreact. Mast cells in your conjunctiva (the thin layer covering your eyeball) release histamine, a chemical that makes blood vessels swell and nerves scream. That’s why your eyes itch, turn red, and water nonstop.Unlike pink eye caused by a virus or bacteria, allergic conjunctivitis doesn’t produce thick yellow or green discharge. You’ll see clear, watery tears. And here’s the key difference: if your eyes are burning and itching more than they’re gunky, it’s likely allergies-not an infection.
Studies show 92% of people with eye allergies report intense itching. Redness hits 88%. Swollen eyelids? That’s 76%. If you’ve got two or more of these symptoms, especially when pollen counts spike, you’re looking at allergic conjunctivitis. The European Academy of Allergy and Clinical Immunology says that’s the diagnostic threshold.
Why Antihistamine Eye Drops Are the Go-To Fix
When your eyes are screaming for relief, antihistamine eye drops are often the fastest answer. They block histamine from binding to nerve endings, which stops the itch before it starts. But not all drops are created equal.First-generation drops like Naphcon-A (pheniramine) work fast-sometimes in under 5 minutes. But they wear off quickly. You’ll need to reapply every 4 to 6 hours. And about 25% of users feel a sharp sting when they drop it in. Not ideal if you’re already in pain.
Second-generation drops like olopatadine (Pataday), ketotifen (Zaditor), and epinastine (Elestat) are smarter. They don’t just block histamine-they also stabilize mast cells, so fewer allergens trigger the reaction in the first place. That’s called dual-action. And they last longer. Pataday Once Daily Relief works for up to 16 hours. That means one drop in the morning, and you’re good until bedtime.
Real-world data backs this up. In clinical trials, olopatadine 0.2% reduced itching scores from 2.8 to 0.7 on a 4-point scale within just 3 minutes. That’s not placebo-it’s measurable relief. Ketotifen works almost as fast, but it doesn’t last as long. By 16 hours, olopatadine users still had itching scores around 0.8, while ketotifen users were up to 1.5. That’s the difference between manageable and miserable.
Cost, Brands, and What Actually Works
Price matters. A lot.Generic ketotifen (the active ingredient in Zaditor) costs about $13 for a 2.5mL bottle at most U.S. pharmacies. Brand-name Pataday? Around $43 for the same size. If you’re paying out of pocket, the generic is a no-brainer. But here’s the catch: if you have insurance, prescription Pataday often costs just $15-$40 as a tier 2 copay. That’s cheaper than the OTC version.
On Amazon and Reddit, users consistently rank Pataday as the most effective for severe symptoms. One verified review says: “Works within minutes and lasts all day.” But another says: “Zaditor is great for budget shoppers, but I need to reapply by noon.”
And don’t be fooled by redness-reducing drops like Visine-A. They contain decongestants (tetrahydrozoline) that shrink blood vessels to make eyes look white. But they don’t touch the itch. Worse, if you use them for more than 3 days, your eyes rebound-becoming redder and more irritated than before. A 2023 study found 65% of users who used them for a week developed this rebound effect. It’s a trap.
What About Oral Antihistamines?
You might think taking Zyrtec or Claritin will fix your eyes too. And yes, they help with sneezing and runny nose. But for your eyes? Not so much.Oral antihistamines can dry out your eyes. In fact, 40% of users in a 2022 study reported worsening dryness, which makes eye allergies feel even worse. Dry eyes and allergic eyes often look the same-red, burning, gritty. But they need totally different treatments. If you’re on an oral antihistamine and your eyes still feel like sandpaper, you might actually have dry eye disease, not allergies.
When You Need More Than Drops
If antihistamine drops aren’t cutting it after 2 weeks, it’s time to dig deeper.For severe cases, doctors may prescribe corticosteroid drops like loteprednol. They work fast-really fast. But they’re not for long-term use. After 2 weeks, 5-10% of users develop higher eye pressure. Left unchecked, that can lead to glaucoma. And prolonged use increases cataract risk. These are powerful tools, but they’re like a fire extinguisher-not a sprinkler system.
The only treatment that actually changes the course of your allergies? Immunotherapy. Allergy shots or sublingual tablets train your immune system to stop reacting. It takes 6-12 months to start working, and you need 3-5 years to see full results. But 60-80% of people report major improvement. If you’ve had eye allergies since childhood and they’re getting worse every spring, this might be your long-term answer.
What You Can Do Right Now
Medication helps-but it’s not the whole story. The best strategy combines drops with smart habits.- Wash your face and hands after being outside. Pollen sticks to skin and hair. A simple rinse can cut symptoms by 30%.
- Use preservative-free artificial tears 4-6 times a day. They flush out allergens before they trigger a reaction.
- Wear wraparound sunglasses outdoors. A 2023 trial showed they block up to 50% of pollen from hitting your eyes.
- Keep windows closed during peak pollen hours (5 a.m. to 10 a.m.). Use AC instead.
- Change your pillowcase every 2-3 days. Dust mites love old fabric.
And here’s the trick most people miss: how you put in the drops. Don’t just squeeze it into your eye. Tilt your head back, pull down your lower lid to make a little pocket, and let one drop fall in. Don’t let the bottle touch your eye. That reduces contamination risk by 75%.
What’s Next in Eye Allergy Treatment?
The field is evolving fast. In 2023, the FDA approved bepotastine 1.5% (Bepreve) as a new once-daily option. It matches olopatadine in effectiveness but with fewer side effects.Even more exciting? An experimental implant called OTX-ALL that releases medication slowly for up to 3 months. It’s in Phase 3 trials and could be a game-changer for people who forget to take drops.
Researchers are also testing biologic drugs that target specific inflammation signals like IL-4 and IL-13. These could be the future-precision treatments tailored to your immune profile.
But for now, the gold standard remains: antihistamine-mast cell stabilizer combos. Dr. David A. Grieshaber, an ophthalmologist in Bern, says it best: “Ketotifen and olopatadine are the current best tools we have.”
When to See a Doctor
If your eyes still feel awful after 2 weeks of proper drop use, it’s not just stubborn allergies. About 20% of people diagnosed with eye allergies actually have dry eye disease, blepharitis, or another condition hiding behind the symptoms. A simple eye exam can rule those out.Also, if you notice vision changes, pain, or light sensitivity beyond normal tearing, don’t wait. These aren’t typical allergy signs. They need urgent attention.
And if you’re using decongestant drops daily? Stop. Now. Talk to your doctor. You’re likely stuck in a cycle of rebound redness.
Can eye allergies cause permanent damage?
No, eye allergies themselves don’t cause permanent damage. But chronic rubbing can scratch the cornea, and long-term use of decongestant drops can lead to rebound redness that’s hard to treat. Corticosteroid drops, if misused, can increase eye pressure and risk cataracts. The key is treating symptoms properly-not ignoring them or overusing quick fixes.
Are antihistamine eye drops safe for long-term use?
Yes, second-generation antihistamine-mast cell stabilizer drops like olopatadine and ketotifen are safe for daily, long-term use. They don’t cause rebound effects or dependency. Many patients use them seasonally for years without issues. Avoid first-generation drops and decongestants for extended use.
Why do my eyes feel worse in the morning?
Pollen counts are highest in the early morning, especially between 5 a.m. and 10 a.m. Also, allergens like dust mites collect on your pillow. If you sleep with windows open or don’t wash your face before bed, allergens sit on your skin overnight. Wash your face and use preservative-free tears before bed to rinse them off.
Can children use antihistamine eye drops?
Yes, but only certain ones. Ketotifen (Zaditor) is approved for kids 3 and older. Olopatadine (Pataday) is approved for children 2 and up. Always check the label or ask your doctor. Never use adult formulations without pediatric approval.
Is there a natural remedy that actually works?
Cold compresses help reduce swelling and soothe itching. A clean, chilled washcloth over closed eyes for 5-10 minutes can provide temporary relief. Artificial tears (preservative-free) flush out allergens. But nothing replaces targeted medication for moderate to severe symptoms. Avoid herbal drops or home remedies-they’re unregulated and can irritate your eyes further.
Eye allergies are common, frustrating, and often misunderstood. But they don’t have to control your life. With the right drops, smart habits, and knowing when to call a doctor, you can stop the itch, clear the redness, and breathe easier-even during peak allergy season.





Write a comment
Your email address will be restricted to us