RA Treatment Effectiveness Calculator
Treatment Options
This tool helps you understand how different treatments work based on your individual situation.
When you're living with rheumatoid arthritis (RA), the goal isn't just to manage pain-it's to stop the damage before it steals your mobility. That’s where DMARDs and biologics come in. These aren’t just pills you take; they’re tools that reprogram your immune system. But how do they work together? And why does mixing them matter more than you think?
What DMARDs Actually Do
Disease-modifying antirheumatic drugs (DMARDs) are the backbone of RA treatment. The most common one, methotrexate, has been used since the 1980s. It’s cheap-often under $50 a month-and it works by slowing down your immune system’s overactive response. But it doesn’t just calm things down; it actually changes the course of the disease. Studies show that about 20-30% of early RA patients reach remission with methotrexate alone. Other traditional DMARDs like sulfasalazine, hydroxychloroquine, and leflunomide work differently but aim for the same result: reduce inflammation before it destroys joints. They’re taken as pills, usually once a day or once a week. Easy to use, but not always easy to tolerate. About 20-30% of people can’t stick with methotrexate because of nausea, fatigue, or liver stress. That’s where things get complicated.Biologics: Precision Tools, Higher Price Tag
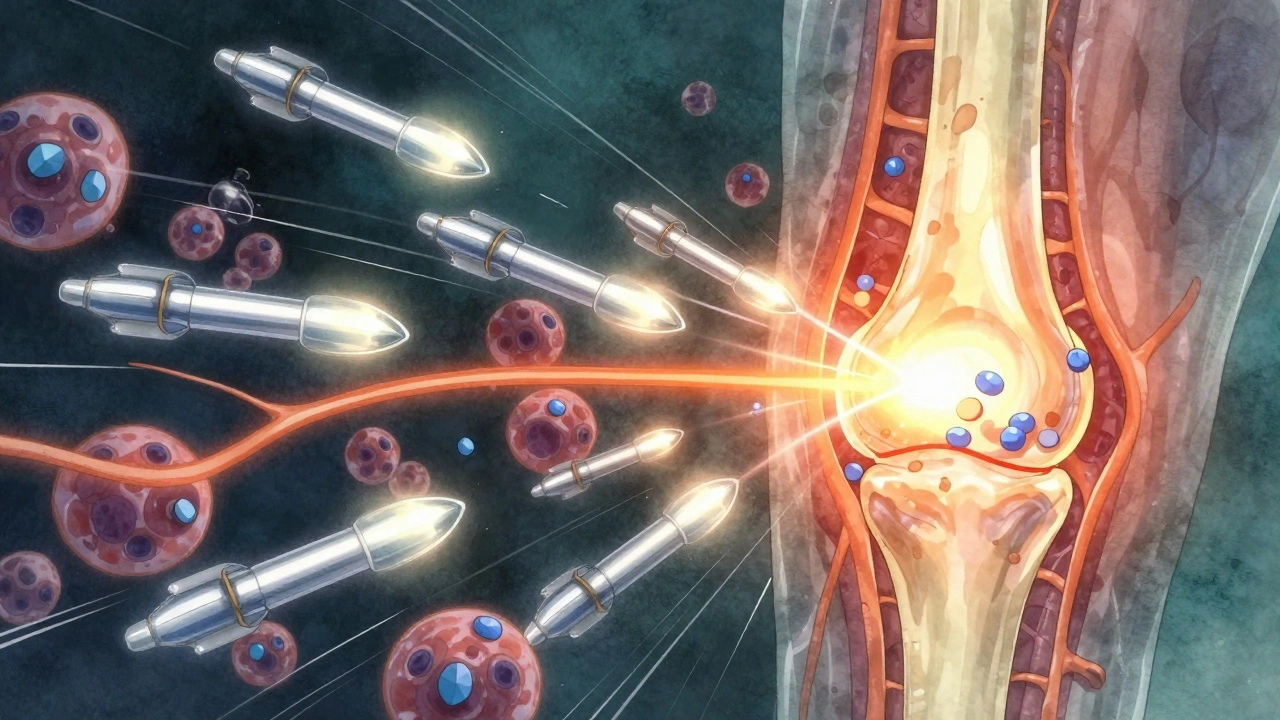
Biologics are different. They’re not chemicals made in a lab-they’re proteins grown in living cells. Think of them like smart missiles targeting specific parts of your immune system. One group, like adalimumab and etanercept, blocks TNF-alpha, a major inflammation signal. Another, like rituximab, wipes out certain B cells. Tocilizumab shuts down IL-6, another key player in joint damage. These drugs don’t come in pill form. You inject them under your skin or get them through an IV. That means more steps, more training, and more cost. A single dose of a biologic can run $1,500 to $6,000 a month. That’s why most doctors start with methotrexate first. But if your RA is aggressive-high antibody levels, early joint erosion, or severe pain-waiting months to add a biologic might mean losing more joint function.Why Combining DMARDs and Biologics Works Better
Here’s the key point most patients miss: biologics work better when paired with methotrexate. A 2015 study in the Journal of Managed Care & Specialty Pharmacy found that when patients took methotrexate along with a biologic, their chance of hitting a 50% improvement in symptoms (called ACR50) jumped from 30-40% to 50-60%. That’s not a small boost-it’s the difference between feeling okay and feeling like yourself again. Methotrexate doesn’t just add power; it helps your body accept the biologic. Without it, your immune system can start making antibodies against the biologic drug, making it less effective over time. That’s why doctors rarely prescribe biologics alone unless you can’t take methotrexate at all. Some patients try to avoid methotrexate because of side effects. But here’s what works: taking folic acid (5-10 mg daily) cuts nausea and fatigue by nearly half. Splitting the methotrexate dose into two smaller doses over the week also helps. And switching from oral to subcutaneous injection can make it easier to tolerate.When Monotherapy Makes Sense
Not everyone needs both. In Switzerland, about one-third of RA patients on biologics take them alone. Why? Mostly because methotrexate didn’t work for them-or they couldn’t handle it. Some people have liver issues. Others get too sick from the nausea. In those cases, biologics like abatacept or rituximab can be used solo. But here’s the catch: monotherapy with biologics is less effective than combination therapy. And it’s way more expensive. A 2022 patient survey found that 41% of people on biologics struggled with cost, and 28% skipped doses because they couldn’t afford them. That’s why biosimilars-cheaper copies of brand-name biologics-are changing the game. Since 2016, biosimilars like Amjevita (a copy of Humira) have cut prices by 15-30%. Now, nearly 28% of the U.S. biologic market is made up of these generics.JAK Inhibitors: The New Oral Option
If you hate needles and can’t tolerate methotrexate, JAK inhibitors might be your best bet. These are small-molecule drugs-taken as pills-that block internal signals that trigger inflammation. Tofacitinib, baricitinib, and upadacitinib fall into this category. Upadacitinib (Rinvoq) was approved in 2023 for early RA as a standalone treatment, matching methotrexate’s effectiveness in trials. But there’s a warning. The FDA added a black box warning to all JAK inhibitors after the 2022 ORAL Surveillance trial showed higher risks of serious infections, heart attacks, and cancer in patients over 50. That doesn’t mean you can’t use them-it means you need to weigh risks. If you’re young, healthy, and have uncontrolled RA, the benefit may outweigh the risk. If you’re older or have a history of heart disease or smoking, your doctor might hold off.Real-World Decisions: What Patients Actually Choose
Online forums tell a different story than clinical trials. On Reddit’s r/rheumatoidarthritis, 63% of 147 respondents said they preferred biologic + methotrexate combos, even with side effects. Why? “Better disease control,” they wrote-87 times. Meanwhile, 37% chose monotherapy, mostly because methotrexate made them too tired or sick. In places like India, cost forces decisions. RA treatment there often starts with a combo of three traditional DMARDs-methotrexate, sulfasalazine, and hydroxychloroquine-because biologics cost 300-500% of a monthly household income. That’s not a luxury; it’s a survival choice.
Monitoring and Safety: What You Need to Know
All biologics and JAK inhibitors require monitoring. Before starting, you’ll need a TB test. You’ll also need blood work every 3-6 months to check liver function, blood counts, and infection markers. TNF inhibitors carry a higher risk of serious infections-like pneumonia or sepsis-so if you get a fever that won’t go away, call your doctor immediately. Injection site reactions are common but usually mild: redness, itching, or swelling. If it turns into a hard lump or gets worse, talk to your nurse. Most people learn to self-inject after one or two training sessions. Specialty pharmacies handle delivery and support, and many offer free nursing visits to walk you through it.What’s Next in RA Treatment
The future is moving toward precision. New drugs are targeting GM-CSF, a different inflammation pathway. Deucravacitinib, a more selective JAK inhibitor, is in late-stage trials and may offer fewer side effects. Ultrasound is now being used to measure remission-not just how you feel, but whether inflammation is truly gone in the joints. The 2024 draft guidelines from the American College of Rheumatology now include ultrasound remission as a goal. That’s a big shift. It means treatment isn’t just about pain relief anymore-it’s about stopping damage at the tissue level.Choosing Your Path
There’s no one-size-fits-all. If you’re newly diagnosed, start with methotrexate. Give it three to six months. If you’re still in pain, swollen joints, or high inflammation markers, add a biologic. If you can’t take methotrexate, try a JAK inhibitor or a biologic alone. If cost is an issue, ask about patient assistance programs. Many drugmakers cover 30-50% of out-of-pocket costs. Biosimilars are widely available now and just as effective. And don’t ignore folic acid-it’s simple, safe, and helps you stay on your medication. The goal isn’t to take the most drugs. It’s to take the right ones-so you can keep moving, working, and living without constant pain.Can I take biologics without methotrexate?
Yes, but it’s usually less effective and more expensive. Biologics work best when combined with methotrexate because methotrexate helps your body tolerate the biologic and boosts its effectiveness. You might skip methotrexate only if you can’t tolerate it due to side effects like nausea, liver issues, or severe fatigue. In those cases, doctors may prescribe a biologic alone, such as abatacept or rituximab.
Why are biologics so expensive?
Biologics are made from living cells using complex processes, which makes them far more expensive to produce than traditional pills. They also require special storage, handling, and delivery systems. A single month’s supply can cost $1,500-$6,000. Biosimilars-copies of brand-name biologics-are now available and can reduce costs by 15-30%. Many patients qualify for financial assistance programs that cover a large portion of the cost.
Do JAK inhibitors have more risks than biologics?
Yes, JAK inhibitors carry a black box warning from the FDA for serious infections, heart problems, blood clots, and certain cancers, especially in patients over 50 or those who smoke. Biologics also increase infection risk, but JAK inhibitors have shown higher rates of major cardiovascular events in long-term studies. That doesn’t mean they’re unsafe-they’re powerful tools-but they require careful screening and regular monitoring. Your doctor will weigh your age, health history, and RA severity before prescribing one.
How long does it take for DMARDs and biologics to work?
Traditional DMARDs like methotrexate can take 6-12 weeks to show noticeable improvement. Biologics usually work faster-some patients feel better in 2-4 weeks, with full effects by 12 weeks. JAK inhibitors fall in between, often showing results in 2-6 weeks. Patience is key, but if you don’t see any change after 3 months, talk to your doctor about adjusting your treatment plan.
Can I stop taking these medications if I feel better?
Stopping medication-even if you feel great-is risky. RA is a chronic condition, and stopping treatment often leads to flare-ups, sometimes worse than before. Some patients in remission may reduce their dose under close supervision, but completely stopping usually brings back inflammation and joint damage. Always work with your rheumatologist before making any changes.
Are there natural alternatives to DMARDs and biologics?
Diet, exercise, and supplements like fish oil or turmeric may help reduce inflammation and improve how you feel, but they don’t stop joint damage like DMARDs and biologics do. There’s no scientific evidence that any natural remedy can replace these medications in halting RA progression. Using them instead of prescribed treatment can lead to permanent joint deformity and disability. Always talk to your doctor before adding supplements, as some can interfere with your medications.
If you’re struggling with side effects, cost, or confusion about your treatment, reach out to your rheumatology team. You’re not alone-specialty pharmacies, patient advocates, and support groups exist to help you navigate this. The right combination isn’t just about science; it’s about what fits your life.


Write a comment
Your email address will be restricted to us