Antimalarial Drug Interaction Risk Calculator
Calculate Your Risk
When you take an antimalarial drug, you’re not just fighting malaria-you’re also managing a hidden risk that can stop your heart. It’s not science fiction. It’s real. Every year, millions take drugs like hydroxychloroquine or artemether-lumefantrine to prevent or treat malaria. But behind the effectiveness of these medicines lies a quiet danger: QT prolongation and CYP enzyme interactions. These aren’t just buzzwords. They’re life-or-death factors that doctors must weigh before prescribing.
What QT Prolongation Really Means
Your heart beats because of electrical signals. These signals travel through chambers, telling them when to contract and relax. The QT interval on an ECG measures how long it takes for your heart’s ventricles to recharge after each beat. If that interval gets too long, your heart can slip into a dangerous rhythm called Torsades de Pointes (TdP). It’s rare, but when it happens, it can kill you in minutes. Some antimalarials directly interfere with the ion channels that control this recharge phase. Chloroquine and hydroxychloroquine block the hERG potassium channel (I_Kr), the same channel targeted by drugs like erythromycin and cisapride-medicines that were pulled from the market because of heart risks. Mefloquine does the same. Lumefantrine, paired with artemether in the most common malaria treatment today, has a half-life of 3 to 6 days. That means it sticks around, building up in your system. And with each dose, the risk climbs. The numbers don’t lie. Studies show that a QTc increase over 500 milliseconds-or more than 60 ms from your baseline-is a red flag. In people with existing heart conditions, older adults, or those on multiple medications, even small delays can tip the balance. The FDA added QT prolongation warnings to hydroxychloroquine labels back in 2011. The European Medicines Agency did the same for lumefantrine in 2015. This isn’t theoretical. It’s documented, reviewed, and confirmed.How CYP Enzymes Turn Safe Drugs Into Dangerous Ones
Your liver uses enzymes-mainly from the CYP family-to break down drugs. CYP3A4 is the most common. It handles about half of all medications you take. Now imagine two drugs that both rely on CYP3A4. They fight for space. One blocks the enzyme. The other can’t get broken down. Result? Toxic buildup. Artemether is metabolized by CYP3A4 into dihydroartemisinin (DHA), its active form. But if you’re taking a CYP3A4 inhibitor-like clarithromycin, ketoconazole, or some HIV protease inhibitors-your body can’t convert artemether properly. That might sound bad, but here’s the twist: artemether itself still has some antimalarial effect. So the risk isn’t always clear-cut. The Northern Alberta HIV Program says: “Likely not clinically significant, but data lacking.” That’s not reassuring. It’s a warning wrapped in uncertainty. Hydroxychloroquine is even more complicated. It’s broken down by CYP2C8, CYP3A4, and CYP2D6. That means it can interact with a wide range of drugs: statins, antidepressants, antifungals, even some antibiotics. A 2021 study by Choi et al. found 12 drugs that, when taken with hydroxychloroquine, dramatically increase QT prolongation risk. Clarithromycin? Odds ratio of 17.85. That’s not a coincidence. That’s a red alarm. Piperacillin/tazobactam, furosemide, and others also showed strong signals-even though they don’t usually prolong QT on their own. Together? Dangerous.Which Antimalarials Are Riskiest?
Not all antimalarials are created equal when it comes to heart risk. Here’s how they stack up:| Drug | QT Risk Level | Primary Mechanism | CYP Interaction Risk |
|---|---|---|---|
| Halofantrine | Very High | Strong hERG block | High (CYP3A4) |
| Lumefantrine | High | hERG inhibition | High (CYP3A4) |
| Chloroquine | Moderate | I_Kr, I_Ca-L, I_KATP block | Moderate (CYP2C8, CYP3A4, CYP2D6) |
| Hydroxychloroquine | Moderate to High | I_Kr block, long half-life | High (CYP2C8, CYP3A4, CYP2D6) |
| Mefloquine | Moderate | hERG inhibition (IC50 ~10 μM) | Low to Moderate |
| Artemether | Low | Minimal direct effect | High (CYP3A4 substrate/inducer) |
| Atovaquone-proguanil | Low | None on hERG | High (mitochondrial interaction) |
Halofantrine is the worst. It’s rarely used today because of its history of causing TdP. But lumefantrine? It’s in the most common treatment worldwide. That’s why clinicians must check for interactions before prescribing artemether-lumefantrine. If a patient is on a protease inhibitor for HIV, or a strong antifungal like itraconazole, the combination could be unsafe.
Who’s Most at Risk?
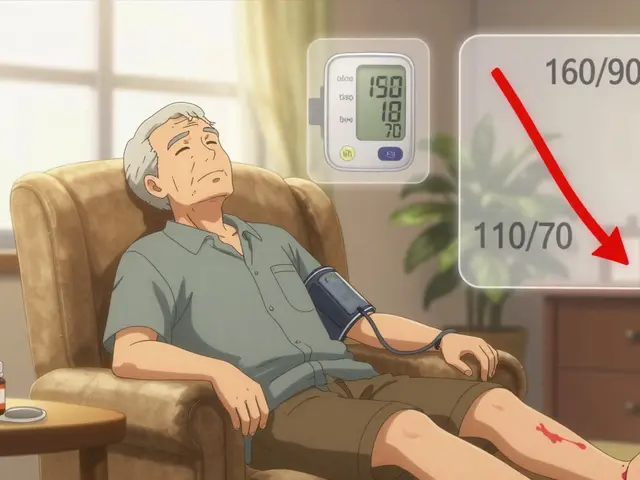
It’s not just about the drug. It’s about the person. Older adults are at higher risk. Their livers don’t clear drugs as efficiently. Their hearts are more likely to have underlying disease. A 70-year-old traveler taking hydroxychloroquine for lupus and also on a statin? That’s a ticking clock. People with pre-existing heart conditions-long QT syndrome, heart failure, bradycardia-are more vulnerable. So are those with electrolyte imbalances: low potassium, low magnesium. These are common in people with chronic illness, diuretic use, or poor nutrition. And then there’s the silent group: people taking antimalarials for autoimmune diseases. Hydroxychloroquine is used by an estimated 1.5 million Americans for lupus and rheumatoid arthritis. Many of them are on other medications: antidepressants, blood pressure pills, painkillers. Few realize that their malaria drug could be the hidden trigger for a cardiac event.What You Should Do (Clinician’s Checklist)
If you’re prescribing or taking an antimalarial, here’s what actually matters:- Check the ECG first. Baseline QTc before starting any high-risk antimalarial. Repeat after 1-2 weeks if on long-term therapy.
- Review all meds. Don’t just look at prescriptions. Include OTC drugs, supplements, and herbal products. Even St. John’s wort can induce CYP3A4 and reduce artemether’s effectiveness.
- Avoid known dangerous pairs. Never combine hydroxychloroquine with clarithromycin, azithromycin (yes, even this one), fluconazole, or certain antipsychotics. Choi et al.’s list of 12 is non-negotiable.
- Watch for signs. Dizziness, palpitations, fainting-these aren’t just “side effects.” They could be early warning signs of TdP.
- Use IV artesunate in emergencies. If someone has severe malaria, intravenous artesunate is the gold standard. Its short half-life means less time for interactions to build up.
- Monitor CBC with sulfadoxine-pyrimethamine. Especially if the patient is also on zidovudine. Bone marrow suppression is real.
There’s no magic formula. But if you skip the ECG, ignore the drug list, and assume “it’s just malaria,” you’re playing Russian roulette with someone’s heart.

Why This Matters More Than Ever
Malaria isn’t going away. In 2021, there were 247 million cases and nearly 620,000 deaths worldwide. Artemisinin resistance, first seen in Cambodia in 2008, is spreading. That means we’re using more combination therapies-and more of the drugs with the worst interaction profiles. The WHO expects current antimalarials to remain the backbone of treatment through at least 2030. That means millions more people will be exposed to these risks. Mass drug administration programs in Africa and Southeast Asia are scaling up. We can’t afford to overlook cardiac safety when giving drugs to entire communities. And here’s the irony: the same drugs we use to save lives from malaria are the ones that can take them away-if we don’t pay attention. The science is clear. The guidelines exist. The warnings are out there. What’s missing is consistent action.What’s Next?
Researchers are building better risk models. Choi et al.’s 2021 study used electronic health records to spot dangerous combinations before they caused harm. That’s the future: predictive, data-driven, automated alerts in prescribing systems. New antimalarials are in the pipeline. But until they’re widely available, we’re stuck with the ones we have. And those come with strings attached. The bottom line? Antimalarials are powerful. But they’re not simple. They’re not safe by default. They’re tools-and like any tool, they can cut both ways. The difference between life and death often comes down to one question: Did someone check the interactions?Can I take hydroxychloroquine with antibiotics?
Some antibiotics are safe, others are dangerous. Clarithromycin and azithromycin significantly increase the risk of QT prolongation when taken with hydroxychloroquine. The odds of a dangerous heart rhythm jump by nearly 18 times with clarithromycin. Ciprofloxacin and levofloxacin also carry some risk. Amoxicillin and doxycycline are generally safer choices, but always check with your doctor before combining any antibiotics with antimalarials.
Is artemether-lumefantrine safe if I’m on HIV meds?
It’s risky. Many HIV medications, especially protease inhibitors like ritonavir and lopinavir, strongly inhibit CYP3A4. This can slow down how your body breaks down artemether and lumefantrine, increasing their levels in your blood. While artemether itself still has some effect, the buildup of lumefantrine raises your QT prolongation risk. The Northern Alberta HIV Program advises caution. If possible, use an alternative antimalarial like atovaquone-proguanil. If artemether-lumefantrine is the only option, monitor ECG closely and avoid high doses.
How often should I get an ECG if I’m on hydroxychloroquine long-term?
For people taking hydroxychloroquine for autoimmune conditions, guidelines recommend a baseline ECG before starting. Then, repeat every 6 to 12 months if you’re under 60 and have no heart disease or other risk factors. If you’re over 60, have kidney disease, diabetes, or are on other QT-prolonging drugs, get an ECG every 3 to 6 months. Any new symptoms-dizziness, skipped beats, fainting-require immediate testing.
Can I take malaria pills if I have a pacemaker?
Having a pacemaker doesn’t automatically make antimalarials safe. Pacemakers help with slow heart rates, but they don’t prevent Torsades de Pointes. In fact, some antimalarials can still trigger dangerous rhythms even with a pacemaker in place. If you have a pacemaker and need malaria prophylaxis, avoid high-risk drugs like lumefantrine or halofantrine. Atovaquone-proguanil or doxycycline are safer options. Always inform your cardiologist before starting any antimalarial.
Are there any antimalarials with no heart risks?
Atovaquone-proguanil (Malarone) has the lowest known risk for QT prolongation. It doesn’t block cardiac ion channels like hERG. However, it does interact with drugs that affect mitochondrial function-like metformin or certain antivirals-and may reduce effectiveness if taken with certain antacids. Doxycycline is another low-risk option for prophylaxis. Neither is perfect, but they’re safer for people with heart conditions or those on multiple medications.
What should I do if I feel dizzy while taking an antimalarial?
Stop taking the medication immediately and seek medical attention. Dizziness, palpitations, or fainting could be signs of a dangerous heart rhythm. Don’t wait. Call your doctor or go to the ER. Bring a list of all your medications, including supplements. An ECG will be needed right away. Even if it’s your first time feeling this way, don’t assume it’s just a side effect. QT prolongation can progress silently until it’s too late.




Write a comment
Your email address will be restricted to us