Chronic heartburn isn’t just annoying-it can change the lining of your esophagus in ways that put you at risk for a rare but deadly cancer. If you’ve had acid reflux for more than 10 years, especially if you’re a man over 50, you might have something called Barrett’s esophagus. It doesn’t cause new symptoms. You won’t feel it. But it’s there, silently changing your cells. And if left unchecked, it can lead to esophageal adenocarcinoma, a cancer with a survival rate below 20% after five years.
What Exactly Is Barrett’s Esophagus?
Barrett’s esophagus happens when the normal tissue lining your esophagus-soft, pink, squamous cells-gets replaced by tougher, salmon-colored columnar cells that look like the lining of your intestine. This change is called intestinal metaplasia. It’s not cancer. It’s not even dysplasia. But it’s a warning sign. Your body is trying to protect itself from the constant burn of stomach acid. Instead of healing properly, it swaps one type of cell for another that’s more resistant to acid. That’s the trade-off. This process doesn’t happen overnight. It takes at least 10 years of frequent acid reflux to trigger it. And once it starts, it doesn’t go away on its own. About 5.6% of people in the U.S. have it. Among those with long-term GERD, the number jumps to 10-15%. Men are three times more likely to develop it than women. White men with a history of smoking and obesity are at the highest risk. The condition is rare in people under 40, and the average age at diagnosis is 62.Why Screening Matters-Even If You Feel Fine
Here’s the hard truth: Barrett’s esophagus has no symptoms of its own. If you have it, you’ll only notice the GERD symptoms you’ve already lived with-heartburn after meals, regurgitation at night, a sour taste in your mouth, trouble swallowing thick foods. Many people assume these are just part of aging or bad eating habits. They don’t get checked. The Esophageal Cancer Action Network found that 68% of people with Barrett’s had symptoms for over five years before diagnosis. That delay can be deadly. Screening isn’t for everyone. The American College of Gastroenterology recommends upper endoscopy only for men who have had frequent GERD (at least weekly) for five years or more, and have at least one other risk factor: age over 50, White race, obesity (especially belly fat), or a history of smoking. Women and younger men without additional risks are generally not screened. Why? Because the overall risk of cancer is still low-even with Barrett’s, only about 5% will develop esophageal cancer over their lifetime. Screening is expensive, invasive, and carries small risks. It’s only justified when the benefit clearly outweighs the cost.How Barrett’s Esophagus Is Diagnosed
Diagnosis isn’t based on symptoms or blood tests. It requires an upper endoscopy-a thin, flexible tube with a camera is passed down your throat. The doctor looks for the telltale salmon-colored patches above the stomach junction. But visual inspection isn’t enough. The lining must be biopsied. That’s where the Seattle protocol comes in. During the procedure, the doctor takes four small tissue samples every 1 to 2 centimeters along the abnormal area. That’s usually 12 to 24 biopsies total. Why so many? Because dysplasia-the precancerous change-can be patchy. One missed spot could mean missing the warning sign. The biopsies are sent to a pathologist who looks for intestinal metaplasia. Then they grade it:- Non-dysplastic Barrett’s esophagus (NDBE): No abnormal cell changes. Most common.
- Indefinite for dysplasia: Unclear if cells are abnormal. Needs repeat testing.
- Low-grade dysplasia (LGD): Mild cell changes. Higher risk.
- High-grade dysplasia (HGD): Severe cell changes. Nearly cancer. Requires immediate action.

What Happens After Diagnosis?
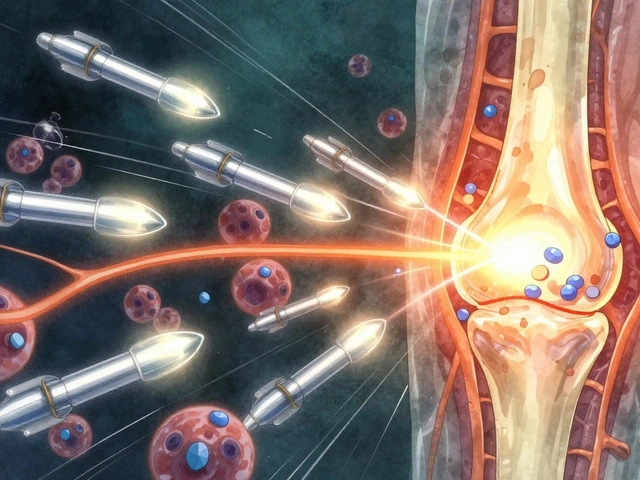
If you’re diagnosed with non-dysplastic Barrett’s, you’re not in immediate danger. But you’re not out of the woods either. The standard is a follow-up endoscopy every 3 to 5 years. You’ll also need to manage your GERD aggressively. That means high-dose proton pump inhibitors (PPIs)-like omeprazole 40 mg twice daily-not just for symptom relief, but to fully suppress acid. Studies show that even if your heartburn feels better, acid may still be refluxing. Only pH monitoring can confirm true suppression. Lifestyle changes are just as important. Lose weight if you’re overweight. Stop smoking. Avoid eating within three hours of bedtime. Elevate the head of your bed by 6 to 8 inches. Cut out fatty foods, chocolate, caffeine, and spicy meals. These aren’t suggestions-they’re part of your cancer prevention plan. If you’re diagnosed with low-grade dysplasia, things get more urgent. The 2022 American Gastroenterological Association guidelines now recommend treating LGD, not just watching it. Endoscopic ablation-using heat (radiofrequency ablation) or cold (cryotherapy)-can remove the abnormal tissue. Success rates are 90-98%. One study showed 77% of patients had no dysplasia left after one year. After treatment, you still need surveillance, but the frequency drops. High-grade dysplasia is treated immediately. Most patients don’t get another endoscopy-they get ablation. The risk of cancer turning up within a year is 6-19%. Waiting is not an option.The Big Problem: Too Many Procedures, Too Few Answers
Here’s the frustrating part: we still can’t predict who will progress to cancer. Of the 5.6% of Americans with Barrett’s esophagus, 95% will never develop cancer. Yet every single one of them needs regular endoscopies. That’s over 1 million procedures a year in the U.S. alone, costing about $1.2 billion annually. Dr. Stuart Spechler from the University of Texas put it bluntly: “The fundamental challenge remains identifying which of the 5.6% of Americans with Barrett’s esophagus will progress to cancer.” New tools are emerging. The TissueCypher Barrett’s Esophagus Assay, approved by Medicare in 2021, analyzes 13 biomarkers from a single biopsy to predict cancer risk with 96% accuracy in ruling out progression. It’s not perfect, but it could cut unnecessary endoscopies by 40%. A $2.4 million study in Texas is testing DNA methylation markers that might one day replace routine biopsies entirely.
What You Should Do If You Have Chronic GERD
If you’ve had heartburn or acid reflux for more than five years, especially if you’re a man over 50, overweight, or smoke:- Don’t assume it’s “just indigestion.”
- Talk to your doctor about an endoscopy. Don’t wait until symptoms get worse.
- If diagnosed with Barrett’s, follow your surveillance schedule. Don’t skip endoscopies.
- Take your PPIs as prescribed-not just when you feel heartburn.
- Make lifestyle changes. Weight loss alone can reduce reflux episodes by 40%.
- Ask about advanced testing like TissueCypher if you have low-grade dysplasia.
Can Barrett’s Esophagus Be Reversed?
Yes. With successful ablation therapy, the abnormal tissue can be eliminated. In many cases, the esophagus regrows normal squamous cells. But you still need lifelong monitoring. The risk of recurrence is real. Even after complete eradication, 10-15% of patients develop Barrett’s again within five years. That’s why surveillance doesn’t stop-it just changes.Final Reality Check
Barrett’s esophagus is a silent threat. It doesn’t scream. It doesn’t hurt in a way that makes you rush to the doctor. But it’s the bridge between a common condition-GERD-and a deadly one-esophageal cancer. The good news? We have tools to catch it early. We have treatments that work. The bad news? Most people don’t know they’re at risk. And many doctors don’t screen the right people. If you’ve had chronic reflux for over a decade, especially with other risk factors, get checked. It’s not about fear. It’s about control. You can’t change your age or your gender. But you can change your habits. And you can ask for the test that might save your life.Can Barrett’s esophagus go away on its own?
No. Once the esophageal lining changes to intestinal metaplasia, it doesn’t revert without treatment. Even if your GERD symptoms improve with medication or lifestyle changes, the abnormal tissue remains. Only endoscopic therapies like radiofrequency ablation can remove it. Without treatment, the risk of progression to cancer remains.
Do proton pump inhibitors (PPIs) prevent cancer in Barrett’s esophagus?
PPIs help control acid and reduce inflammation, but they don’t eliminate cancer risk. Studies show that even with PPIs, acid reflux can still occur in 30-45% of patients. While PPIs are essential for managing symptoms and slowing damage, they’re not a cure. The only proven way to reduce cancer risk is through endoscopic surveillance and ablation of dysplastic tissue.
Is Barrett’s esophagus hereditary?
There’s no single gene that causes Barrett’s, but family history does matter. People with a first-degree relative (parent, sibling) who had Barrett’s or esophageal cancer have a 2-3 times higher risk. This suggests a genetic predisposition, possibly linked to how the body responds to acid or heals tissue. If you have a family history, be proactive about screening.
Can I get screened for Barrett’s esophagus without an endoscopy?
Not yet as a standard. Endoscopy with biopsy is still the gold standard. But new non-endoscopic tests are emerging. The TissueCypher assay uses a swallowable balloon to collect cells from the esophagus, then analyzes biomarkers to assess cancer risk. It’s approved for use in patients already diagnosed with Barrett’s to guide surveillance. It’s not a replacement for initial diagnosis, but it could reduce how often you need an endoscopy in the future.
Why do men get Barrett’s esophagus more often than women?
Men are three times more likely to develop Barrett’s esophagus, and the reasons aren’t fully understood. Hormonal differences may play a role-estrogen may protect women’s esophageal tissue. Men are also more likely to have central obesity, smoke, and delay medical care. Plus, GERD tends to be more severe and persistent in men. The combination of biology and behavior creates a perfect storm.
What happens if I ignore my Barrett’s esophagus diagnosis?
Ignoring it doesn’t mean nothing happens-it means you’re waiting for cancer to develop. Progression from non-dysplastic Barrett’s to cancer usually takes 10-20 years. But once cancer appears, it’s often advanced. Symptoms like trouble swallowing, weight loss, or chest pain show up late. At that stage, treatment is aggressive, survival is low, and recovery is uncertain. Surveillance gives you time to act before it’s too late.
Can I still eat normally if I have Barrett’s esophagus?
You can, but you’ll need to adjust. Fatty foods, chocolate, caffeine, alcohol, citrus, and spicy meals relax the lower esophageal sphincter and trigger reflux. Eating large meals or lying down soon after eating makes it worse. The goal isn’t to eliminate all enjoyment-it’s to reduce triggers. Many people find that after a few weeks of dietary changes, their reflux improves so much they can enjoy more foods without symptoms.
Is Barrett’s esophagus the same as esophageal cancer?
No. Barrett’s esophagus is a precancerous condition. It means the cells have changed in a way that increases cancer risk, but they’re not cancer yet. Think of it like a sunburn that keeps happening-each burn increases the chance of skin cancer. Barrett’s is the same: chronic acid exposure changes the cells, and over time, those changes can turn malignant. Most people with Barrett’s never get cancer-but the risk is real enough to warrant monitoring.



Write a comment
Your email address will be restricted to us