Liver-Heart Risk Assessment Tool
Liver Risk Factors
Factors that harm liver function and increase heart disease risk.
Heart Risk Factors
Factors that harm heart function and increase liver disease risk.
Your Risk Assessment
Recommendations:
When the liver stops working properly, the heart often feels the impact. Understanding the link between liver failure and heart disease can help you spot danger early and take steps to protect both organs.
Key Takeaways
- Liver failure creates systemic inflammation and hormonal imbalances that strain the cardiovascular system.
- Conditions such as cirrhosis, portal hypertension, and metabolic syndrome are major bridges between the liver and heart.
- Shared risk factors-excess alcohol, hepatitis infections, and obesity-fuel both liver and cardiac damage.
- Early detection of symptoms like fluid buildup, abnormal heart rhythm, or sudden fatigue can prevent severe complications.
- Lifestyle changes, targeted medication, and coordinated care between hepatologists and cardiologists improve outcomes.
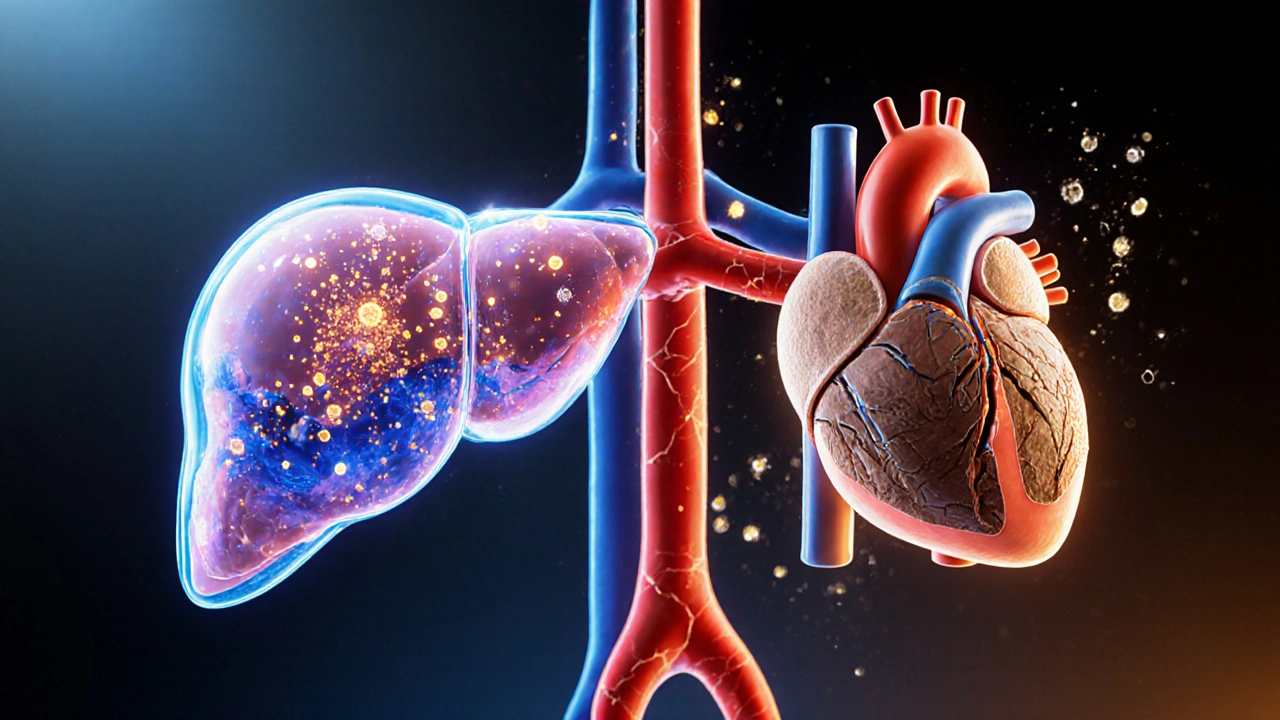
How the Liver and Heart Talk to Each Other
Both organs are part of a tightly knit network that regulates blood flow, hormones, and metabolism. When the liver is healthy, it filters toxins, balances cholesterol, and produces proteins that keep blood pressure stable. When it fails, these functions collapse, and the heart has to pick up the slack.
Liver Failure is the loss of sufficient liver function to sustain normal metabolic processes, often marked by jaundice, coagulopathy, and encephalopathy. The resulting buildup of toxic substances like ammonia and inflammatory cytokines can directly damage heart muscle cells.
Heart Disease is a broad term for conditions that affect the heart’s structure or function, including coronary artery disease, heart failure, and arrhythmias. It frequently emerges as a secondary complication when the liver can’t clear harmful metabolites.
Mechanisms Linking Liver Failure to Heart Disease
Researchers have identified several pathways that turn a sick liver into a cardiac threat:
- Systemic Inflammation: A failing liver releases large amounts of tumor necrosis factor‑alpha (TNF‑α) and interleukin‑6 (IL‑6). These cytokines accelerate atherosclerotic plaque formation and weaken heart muscle contractility.
- Toxin Accumulation: Substances such as ammonia, bilirubin, and endotoxins cross the blood‑brain barrier and also affect myocardial cells, causing arrhythmias and reduced pumping efficiency.
- Hormonal Imbalance: The liver synthesizes angiotensin‑converting enzyme (ACE) regulators and produces insulin‑like growth factor‑1 (IGF‑1). Failure reduces IGF‑1, promoting vascular stiffness and hypertension.
- Hemodynamic Stress: Portal hypertension raises pressure in the portal vein, leading to hyperdynamic circulation. The heart compensates by beating faster and harder, eventually tiring out.
- Coagulopathy: Impaired clotting factors increase both bleeding risk and paradoxical clot formation in coronary arteries, a key trigger for heart attacks.
These mechanisms are not isolated; they interact, creating a vicious cycle where liver dysfunction worsens cardiac health, and cardiac strain further impairs liver perfusion.
Common Risk Factors That Hit Both Organs
Many lifestyle and medical conditions act as shared accelerators. Below is a quick reference of the most impactful factors.
| Risk Factor | Effect on Liver | Effect on Heart |
|---|---|---|
| Excess Alcohol | Alcoholic liver disease, cirrhosis | Cardiomyopathy, hypertension |
| Chronic Hepatitis C | Progressive fibrosis, cirrhosis | Accelerated atherosclerosis, insulin resistance |
| Obesity / Metabolic Syndrome | Non‑alcoholic fatty liver disease (NAFLD) | Elevated LDL, endothelial dysfunction |
| Smoking | Oxidative stress, worsened fibrosis | Increased plaque formation, reduced oxygen delivery |
| Type 2 Diabetes | Impaired glycogen storage, NAFLD | Microvascular disease, higher heart failure risk |
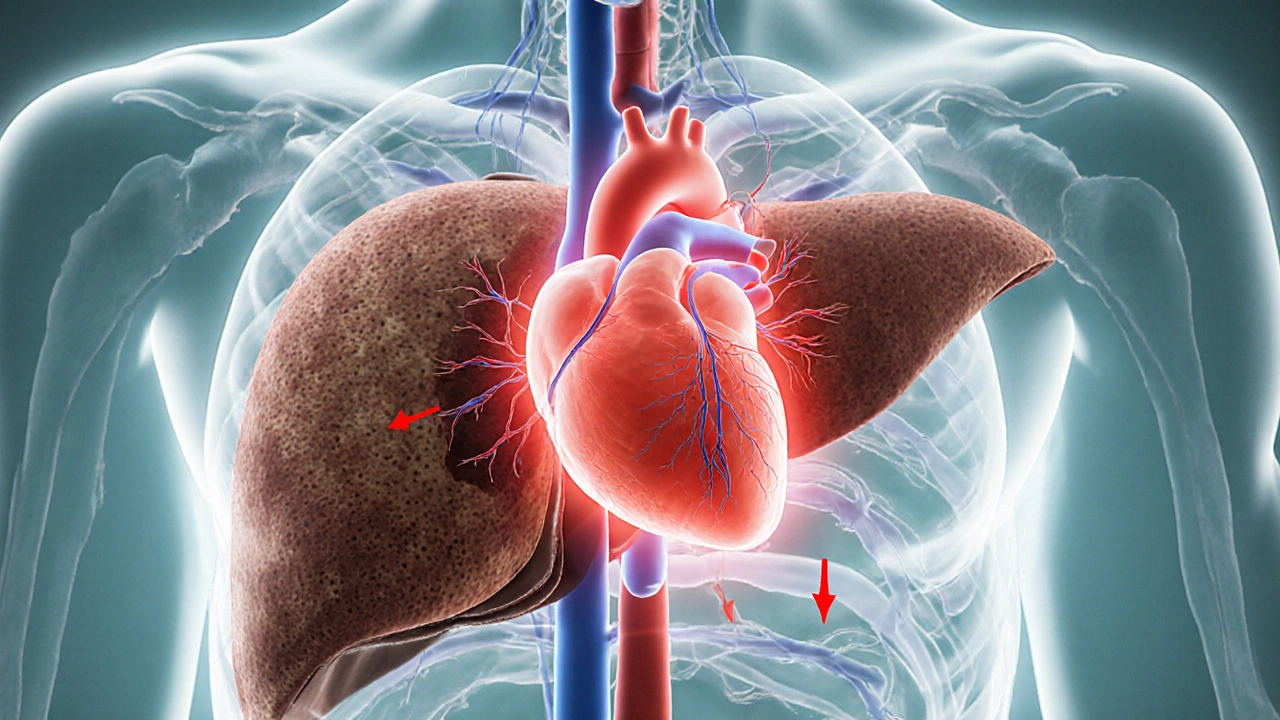
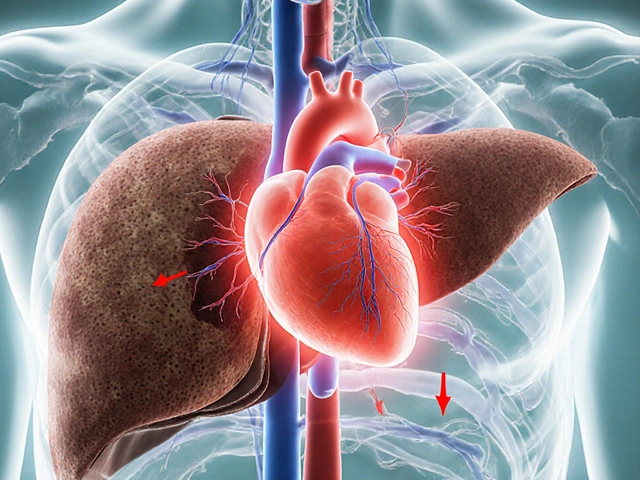
Key Liver Conditions That Boost Cardiac Risk
Understanding specific liver diseases helps you gauge heart danger more accurately.
Cirrhosis is the end‑stage scarring of the liver caused by chronic injury, leading to impaired blood flow and toxin clearance. Cirrhosis often accompanies portal hypertension, which forces the heart to pump against higher vascular resistance.
Portal Hypertension is elevated pressure in the portal venous system, commonly resulting from cirrhosis and causing varices and ascites. The condition triggers a hyperdynamic circulatory state-high cardiac output, low systemic vascular resistance-that can evolve into heart failure.
Cardiomyopathy is a disease of the heart muscle that reduces its ability to pump blood efficiently, sometimes induced by chronic alcohol abuse. When alcohol simultaneously damages the liver, the combined load dramatically raises mortality risk.
Atherosclerosis is the buildup of plaque within arterial walls, narrowing vessels and restricting blood flow. Liver‑derived inflammation accelerates plaque formation, linking liver dysfunction directly to coronary artery disease.
Metabolic Syndrome is a cluster of conditions-including high blood pressure, high blood sugar, excess abdominal fat, and abnormal cholesterol-that increase the risk of heart disease, stroke, and type 2 diabetes. It also fuels non‑alcoholic fatty liver disease, creating a two‑way road to organ failure.
Hepatitis C is a viral infection that can cause chronic liver inflammation, fibrosis, and eventually cirrhosis. Chronic infection raises systemic inflammatory markers that are known drivers of cardiovascular events.
Symptoms to Watch For
Because liver and heart issues can mask each other, look for a mix of signs:
- Unexplained swelling in the legs, ankles, or abdomen (ascites)
- Persistent fatigue despite adequate rest
- Shortness of breath during mild activity
- Yellowing of the skin or eyes (jaundice)
- Irregular heartbeat or palpitations
- Sudden weight gain from fluid retention
- Confusion or memory lapses (hepatic encephalopathy)
If you notice any combination of these, a prompt medical evaluation can catch complications before they become life‑threatening.
Prevention and Management Strategies
Protecting both the liver and heart requires a coordinated approach.
- Limit Alcohol: Keep intake below 14g per day for women and 28g for men. If you already have liver disease, abstinence is best.
- Adopt a Heart‑Healthy Diet: Emphasize leafy greens, berries, whole grains, and fatty fish rich in omega‑3s. Reduce processed sugars and trans fats.
- Maintain a Healthy Weight: Aim for a BMI between 18.5 and 24.9. Even a 5‑% weight loss can reverse early NAFLD and improve insulin sensitivity.
- Control Blood Sugar and Blood Pressure: Regular monitoring and medication adherence lower stress on both organs.
- Vaccinate Against Hepatitis: HepatitisA andB vaccines prevent viral liver damage that can later impact the heart.
- Stay Active: 150 minutes of moderate aerobic exercise per week improves cardiovascular fitness and helps reduce liver fat.
- Regular Screening: People with chronic liver disease should have annual cardiac echo or stress test, while heart patients benefit from liver function panels.
When disease is already present, a multidisciplinary team-hepatologist, cardiologist, nutritionist, and primary care physician-creates a personalized plan that may include diuretics for fluid overload, beta‑blockers to reduce portal pressure, and statins to curb cholesterol buildup.
When to Seek Medical Help Immediately
Emergency signs include:
- Severe chest pain radiating to the arm or jaw
- Sudden shortness of breath or wheezing
- Rapid heart rate (>120bpm) with dizziness
- Profound abdominal pain with swelling
- Confusion, sleepiness, or inability to stay awake
Call emergency services or head to the nearest hospital. Early treatment of heart attack or acute liver decompensation can save lives.
Frequently Asked Questions
Does liver failure always cause heart disease?
No. While liver failure dramatically raises the risk of cardiovascular problems, not every patient develops heart disease. Genetics, lifestyle, and the underlying cause of liver failure influence the outcome.
Can treating heart disease improve liver function?
In some cases, yes. Reducing cardiac workload with medications or surgery can enhance liver perfusion, slowing further hepatic damage. However, direct liver‑targeted therapy remains essential.
Are there medications that protect both organs?
Statins, originally for cholesterol, have been shown to lower inflammation markers in both the liver and arteries. Beta‑blockers help control portal hypertension and reduce heart rate, offering dual benefit for many patients.
How often should someone with cirrhosis see a cardiologist?
At minimum once a year, or sooner if new symptoms (e.g., chest pain, edema) appear. Annual echocardiograms help track early changes.
Is liver transplantation a cure for the heart problems?
Transplant can reverse many liver‑related cardiovascular stresses, but existing heart disease may still need separate treatment. Post‑transplant patients are closely monitored for cardiac function.


Write a comment
Your email address will be restricted to us