Clearing expired medications isn’t just about tidying up a shelf. It’s a safety step that can prevent accidental overdoses, dangerous reactions, or worse-giving someone medicine that’s lost its effectiveness. Every year in the U.S. alone, over 1.3 million emergency room visits are tied to expired or improperly stored drugs, according to the FDA. If you work in a pharmacy, clinic, nursing home, or even manage medications at home, knowing how to properly check lot numbers and recalls before disposal isn’t optional. It’s required.
Why Lot Numbers Matter More Than You Think
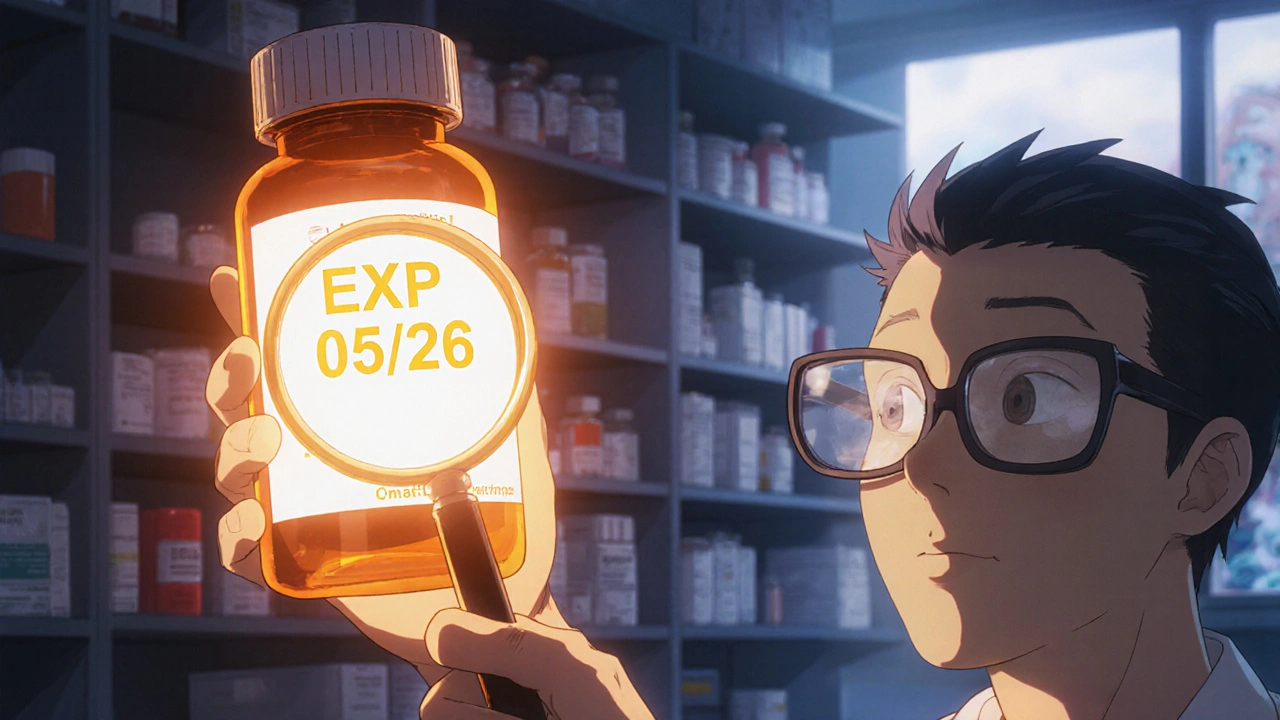
Lot numbers aren’t random codes. They’re traceable identifiers assigned by manufacturers to each batch of medication produced. When a safety issue pops up-a contaminated pill, a mislabeled dose, a degraded ingredient-the lot number is the key that lets regulators and pharmacies pull only the affected units, not every bottle of that drug in the country. The FDA has required lot numbers on all prescription drugs since 1979 under 21 CFR § 211.137. Since 2010, they’ve also required the expiration date (EXP) to be clearly printed alongside it. But here’s the catch: you cannot calculate an expiration date from a lot number. Too many people try. They see "230515" and assume that’s the expiration date. It’s not. That’s usually the manufacturing date. The shelf life? That varies by drug. Some last 2 years. Others, like insulin or liquid antibiotics, expire in 28 days after opening. You can’t guess. You have to read the label.How to Read the Expiration Date (EXP) Correctly
Look for the letters "EXP" followed by a date. That’s your legal expiration. It’s printed on the bottle, box, or blister pack. The format? Usually month/year (like EXP 05/26). But not always. Some international medications use day/month/year (15/05/26). If you’re unsure, assume the first two numbers are the month. If it says EXP 12/24, it expires in December 2024. If it says EXP 24/12, it’s still December 2024. Don’t rely on the lot number. Don’t assume all bottles from the same manufacturer have the same shelf life. Don’t trust memory. Even if you’ve handled this drug for years, the expiration date is the only thing that matters legally and medically. The FDA is clear: the printed EXP date supersedes any calculation you might try to make from the lot number.How to Check for Recalls Using the Lot Number
Once you’ve confirmed the expiration date, you need to check if that specific lot has been recalled-even if it hasn’t expired yet. A drug can be pulled for contamination, mislabeling, or potency issues long before it hits its expiration date. The FDA maintains a public database called Recalls, Market Withdrawals & Safety Alerts. Go to fda.gov/safety/recalls. Search by drug name, manufacturer, or lot number. You can also call the manufacturer directly. Many companies list recall info on their websites under "Drug Safety" or "Patient Support." If you find a match-your lot number is on a recall list-don’t just throw it away. Isolate it. Mark it clearly. Contact your regional FDA office or local health department for proper disposal instructions. Some recalls require you to return the product. Others require special hazardous waste handling.What to Do When Lot Numbers Are Hard to Read
Damaged labels are common. Bottles get knocked around. Boxes get wet. Stickers peel. If the EXP date is faded or missing, here’s what to do:- Check the original packaging or invoice. Many pharmacies keep digital copies of supplier receipts with lot and expiry info.
- Scan the lot number into your inventory system. If you use a pharmacy management system like IFS or MedKeeper, it may pull expiry data from the manufacturer’s database.
- Call the manufacturer. Have the lot number ready. Most have a toll-free number for pharmacists and providers.
- If you can’t confirm the expiry date, treat it as expired. It’s safer to dispose of a good drug than risk giving someone a bad one.

Use Technology to Cut Human Error
Manual checks are slow and error-prone. A 2022 study showed that 12.7% of expiration dates were misread during manual inventory. Automated systems cut that to 0.3%. If your facility uses barcode scanners linked to a database, make sure they’re set up to read both the lot number and the EXP date. New AI tools like Medplore’s scanner can even read expiration dates from blurry or damaged photos with 99.2% accuracy. Even if you don’t have fancy tech, simple steps help. Use bright, 500+ lux lighting when checking labels. Wear reading glasses if needed. Don’t rush. One misread date can lead to a patient getting ineffective antibiotics or a child getting an expired epinephrine auto-injector.Follow the 7-Step Clearance Process
The American Society of Health-System Pharmacists (ASHP) recommends this clear, step-by-step method for clearing expired meds:- Isolate any drug within 60 days of its EXP date.
- Scan or enter the lot number into your inventory system 30 days before expiration.
- Check the FDA recall database using that lot number.
- Confirm with the manufacturer if there are any active recalls or safety notices for that batch.
- Take timestamped photos of the expired items before disposal.
- For controlled substances (like opioids or benzodiazepines), complete FDA Form 3639.
- Keep records for at least two years, as required by the DEA.
Common Mistakes That Put People at Risk
Here’s what goes wrong-and how to avoid it:- Mistake: Assuming "MFG 03/22" means it expires in March 2022. Fix: That’s the manufacturing date. Look for "EXP".
- Mistake: Disposing of a drug because the lot number looks "suspicious." Fix: Only act if there’s an official recall.
- Mistake: Throwing expired meds in the trash without checking local rules. Fix: Many areas require drug take-back programs. Flushing is only allowed for certain high-risk drugs (check fda.gov/drug-disposal).
- Mistake: Not updating manufacturer contact info. Fix: Update your list quarterly. Companies change phone numbers, websites, and recall procedures.
Why Independent Pharmacies Are Falling Behind
Chain pharmacies? Almost all use automated systems. 98.7% of them track lot numbers and expiration dates electronically. But only 42.3% of independent pharmacies do, according to the National Community Pharmacists Association. That’s a dangerous gap. One independent pharmacy in Wisconsin recently kept expired insulin in stock for six months because their staff misread a lot number as an expiry date. A patient nearly died. The fix? Start small. Even a free spreadsheet with columns for drug name, lot number, EXP date, and recall status can cut your error rate in half. Use the FDA’s public database. Train staff for just 4 hours. Three practice runs bring accuracy to 90%.
What’s Changing in 2025 and Beyond
By November 2025, the FDA will require all pharmacies to have full electronic lot tracking. That means no more handwritten logs. No more guesswork. Systems will auto-flag expirations and recalls. The industry is moving toward GS1 standards-uniform barcode formats that make scanning faster and more accurate. AI and blockchain are helping too. Pfizer’s MediLedger project already cut expiry errors by 28% in pilot sites. By 2027, experts predict lot-number-related errors will drop by 95%. But until then, you can’t wait for technology to save you. You need to act now.Final Rule: When in Doubt, Dispose
If you can’t confirm the expiration date, if the label is torn, if the lot number doesn’t match any recall data, or if the pill looks discolored, cracked, or smells odd-dispose of it. Don’t risk it. Medications don’t just "go bad." They can become toxic, ineffective, or even harmful. And remember: disposal isn’t just dumping in the trash. Check your local pharmacy’s take-back program. Many offer free drop-off. If none exist, mix pills with coffee grounds or cat litter, seal them in a container, and throw them in the trash. Never flush unless the label says to.Frequently Asked Questions
Can I use the lot number to find out when my medicine expires?
No. Lot numbers track manufacturing batches, not expiration dates. The only reliable way to know when a medication expires is to read the "EXP" date printed on the packaging. Never guess or calculate based on the lot number.
What should I do if a medication has expired but there’s no recall?
Dispose of it properly. Even if there’s no recall, expired medication can lose potency or break down into harmful compounds. Use a drug take-back program if available. If not, mix it with an unpalatable substance like coffee grounds or cat litter, seal it in a container, and throw it in the trash. Never flush unless instructed.
How often should I check for drug recalls?
Check the FDA’s Recalls, Market Withdrawals & Safety Alerts page at least once a week. If you handle high-risk drugs like insulin, epinephrine, or antibiotics, check daily. Set up email alerts from the FDA or your manufacturer for faster notifications.
Are expired medications dangerous to take?
Some are. Antibiotics may not kill infections, leading to worse illness. Heart medications might not control blood pressure. Epinephrine auto-injectors can fail completely. While not all expired drugs are toxic, you can’t know which ones are still safe. The risk isn’t worth it.
Why do some international medications have different date formats?
Different countries use different date formats. In the U.S., it’s usually month/year. In Europe and many other places, it’s day/month/year. Always check the label carefully. If you’re unsure, assume the first two numbers are the month. When in doubt, contact the manufacturer or consult a pharmacist.
What’s the best way to train staff on checking lot numbers and expirations?
Start with real examples. Show expired bottles with faded labels. Practice scanning lot numbers into your system. Use the FDA recall database for mock checks. Require staff to verify expiration dates aloud before disposal. After three practice cycles, accuracy jumps to 90%. Keep training materials visible and update them quarterly.


Write a comment
Your email address will be restricted to us