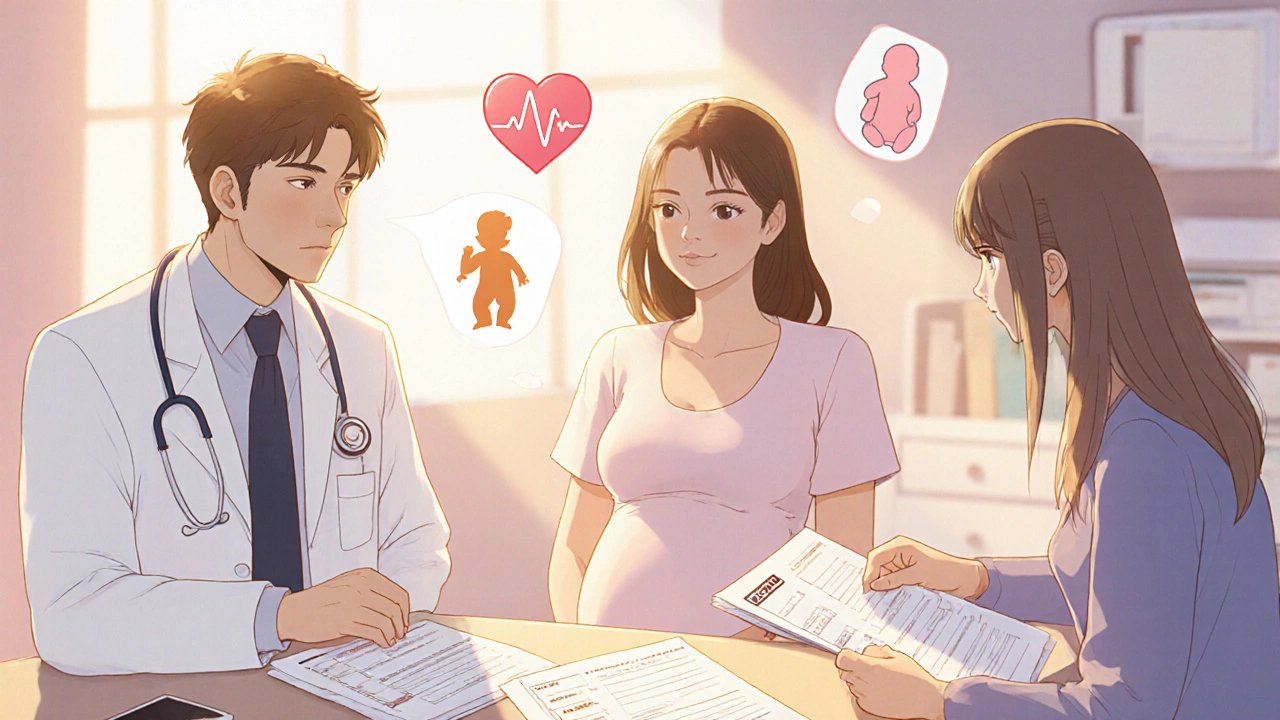
When you're pregnant or breastfeeding and need psychiatric medication, you're not just managing your mental health-you're managing two lives. That’s why coordinating care between your OB/GYN and psychiatrist isn’t optional. It’s essential. Too many women get caught in the middle: one provider says to stay on medication, another says to stop. The result? Unnecessary stress, relapse, or worse-hospitalization. The good news? There’s a clear, evidence-based way to make this work.
Why Coordination Matters More Than Ever
About 1 in 5 women experience depression or anxiety during pregnancy or after birth. Left untreated, these conditions raise the risk of preterm birth by 40%, low birth weight by 30%, and even developmental delays in children. But some medications, if used without proper oversight, carry small but real risks to the baby. The goal isn’t to avoid all meds-it’s to use the right ones, at the right dose, at the right time. The American College of Obstetricians and Gynecologists (ACOG) made this official in 2023: coordinated care reduces medication discontinuation by more than half. Women who see both their OB/GYN and psychiatrist together are 37% less likely to develop severe postpartum depression. That’s not a suggestion-it’s a proven outcome.What Medications Are Safe? The Clear Choices
Not all antidepressants are created equal when you’re pregnant or nursing. The data is clear: sertraline and escitalopram are the first-line choices. Why? - Sertraline has a 0.5% absolute risk increase for heart defects-compared to a 1% baseline risk in the general population. That’s lower than the risk from smoking or uncontrolled anxiety. - Escitalopram has minimal placental transfer and almost no active metabolites, meaning less exposure for the baby. - Both are found in breast milk at very low levels, and studies show no significant impact on infant development. Avoid paroxetine. It’s linked to a higher risk of heart defects. Also avoid valproate if you have bipolar disorder-it carries a 10.7% risk of major birth defects. Lithium is an option but needs close monitoring of kidney and thyroid function. For anxiety, benzodiazepines like lorazepam can be used short-term, but only under weekly psychiatrist supervision. Long-term use increases the risk of neonatal withdrawal.When Should Coordination Start? Timing Is Everything
Waiting until you’re 20 weeks pregnant is too late. The best window is before conception. - If you’re planning pregnancy, schedule a joint visit with both providers 3-6 months ahead. Review your current meds, adjust doses if needed, and document your plan. - If you’re already pregnant, aim for that first coordination meeting by 8-10 weeks. That’s when the baby’s organs are forming, and medication choices matter most. - After birth, keep meetings every 4 weeks for stable cases. If symptoms flare up, schedule weekly check-ins. The National Pregnancy Registry for Psychiatric Medications has tracked over 15,000 pregnancies. Their data shows that women who planned ahead had 60% fewer emergency visits in the postpartum period.
How Do Providers Actually Talk to Each Other?
This is where things break down. In 67% of practices, the OB/GYN’s electronic health record doesn’t talk to the psychiatrist’s system. So how do they coordinate? The answer: standardized templates. ACOG recommends a 12-point safety checklist that includes:- Medication name and dose
- Protein binding percentage (sertraline binds at 98%)
- Placental transfer coefficient
- Lactation risk category (L1 or L2 is safest)
- Half-life (24-48 hours ideal)
- Maternal relapse risk without treatment
- Known fetal risks
- Current trimester
- Recent lab values (e.g., lithium levels)
- Patient’s preference
- Plan for dose adjustment during third trimester
- Follow-up date
What If You’re Already on Meds and Just Found Out You’re Pregnant?
Don’t panic. Don’t stop cold turkey. That’s when relapse is most likely. - Call your OB/GYN immediately. Ask them to reach out to your psychiatrist. - If you’re on paroxetine, switch to sertraline under supervision. It takes 7-10 days to stabilize. - If you’re on multiple psychiatric meds, simplify to one. Polypharmacy increases neonatal complications by 30%. - If you’re on mood stabilizers like lamotrigine, your dose may need to be increased by 50-100% during pregnancy due to faster metabolism. The FDA updated prescribing labels in January 2024 to reflect this. Sertraline’s label now says: “Coordination with obstetric provider recommended for dose adjustment beginning at 20 weeks gestation.” That’s not a footnote-it’s a directive.What About Breastfeeding?
Yes, you can safely breastfeed while taking sertraline or escitalopram. Both pass into breast milk at levels below 1% of the maternal dose. Studies show no effect on infant weight gain, sleep, or development at 6 and 12 months. Avoid fluoxetine. It stays in the system longer and can build up in babies, potentially causing irritability or poor feeding. If you’re worried, ask for a drug level test on your baby’s blood. It’s rare, but available through pediatric pharmacology labs. Most moms don’t need it-just monitor for fussiness, poor feeding, or unusual sleepiness in the first few weeks.
Barriers You Might Face (And How to Beat Them)
You’re not alone if you’ve run into roadblocks: - Insurance delays: 57% of privately insured women wait more than 14 days for prior authorization. Call your insurer daily. Ask for a case manager. Mention ACOG guidelines-they’re now a standard of care. - Provider disconnect: If your OB/GYN says “I don’t know about meds,” ask for a referral to a maternal-fetal medicine specialist or a perinatal psychiatrist. Academic hospitals have these teams. - Conflicting advice: If one provider says “stop,” and another says “keep going,” demand a joint meeting. Bring the ACOG checklist. Use the National Pregnancy Registry’s public data as a reference. Kaiser Permanente’s integrated program saw 89% patient satisfaction because they held joint video visits. You don’t need to go to two offices-you can have both providers on the same call.The Future Is Here: Tech Is Making Coordination Easier
Epic Systems launched its Perinatal Mental Health Module in early 2023. Now, when an OB/GYN prescribes sertraline, the system automatically alerts the patient’s psychiatrist. No more missed messages. No more paperwork delays. In 2024, CMS started rewarding practices that document coordinated care. If 90%+ of your perinatal mental health cases have documented communication between providers, you get a 5% reimbursement bonus. That’s why more clinics are adopting these protocols. The NIH is launching a 5,000-woman study in late 2024 called PACT, which will use genetic testing to predict which meds work best for each woman. That’s the next step: personalized care.What You Can Do Today
1. Ask your OB/GYN: “Do you coordinate with psychiatrists for medication management during pregnancy?” If they say no, ask for a referral. 2. Ask your psychiatrist: “Do you work with OB/GYNs on perinatal cases?” If not, find one who does. 3. Bring the ACOG checklist to your first joint visit. Print it from their website. It’s free. 4. Join the National Pregnancy Registry-it’s free, confidential, and helps future moms. Go to www.nationalpregnancyregistry.org. 5. Don’t stop meds without a plan. Untreated depression is riskier than most medications. This isn’t about being perfect. It’s about being informed. You’re not choosing between your mental health and your baby’s safety-you’re choosing the best way to protect both.Can I take antidepressants while breastfeeding?
Yes, sertraline and escitalopram are considered safest. Both pass into breast milk at very low levels-less than 1% of the mother’s dose. Studies show no negative effects on infant development, weight gain, or sleep patterns at 6 and 12 months. Avoid fluoxetine, as it stays in the system longer and can build up in babies. Always monitor your baby for unusual fussiness, poor feeding, or sleep changes in the first few weeks.
What if my OB/GYN says to stop my medication but my psychiatrist says to keep it?
Demand a joint appointment. This isn’t a disagreement-it’s a coordination failure. Bring the ACOG 2023 guidelines and the National Pregnancy Registry data. Most OB/GYNs aren’t trained in psychopharmacology; most psychiatrists aren’t trained in pregnancy physiology. Both need to see the full picture. ACOG explicitly says OB/GYNs should initiate treatment for perinatal depression and refer when needed. If your providers can’t agree, ask for a referral to a perinatal psychiatry clinic or academic medical center.
Is it safe to stay on mood stabilizers during pregnancy?
It depends. Valproate is dangerous-it raises the risk of major birth defects to 10.7%. Avoid it completely. Lithium is an option but requires monthly blood tests to monitor kidney and thyroid function. Lamotrigine is often preferred because it has a lower risk profile, but your dose may need to be increased by 50-100% during pregnancy due to faster metabolism. Never stop mood stabilizers abruptly. Uncontrolled bipolar disorder increases the risk of preterm birth, suicide, and neonatal complications more than the medication itself.
When should I start coordinating care if I’m planning to get pregnant?
Start 3 to 6 months before conception. This gives time to switch to safer medications if needed, adjust doses, and document your plan. Pregnancy alters how your body processes drugs-plasma volume increases by 40-50%, and liver enzymes become more active. Waiting until you’re pregnant means playing catch-up. Preconception planning reduces emergency visits by 60% in the postpartum period.
Why is sertraline preferred over other SSRIs during pregnancy?
Sertraline has the most extensive safety data from over 15,000 pregnancies tracked by the National Pregnancy Registry. It has high protein binding (98%), which limits placental transfer. It has minimal active metabolites and a half-life of 26 hours-ideal for steady levels during pregnancy. It’s also the only SSRI with FDA labeling that specifically recommends coordination with an OB/GYN at 20 weeks. Paroxetine has a higher risk of heart defects. Fluoxetine stays in the system too long. Escitalopram is a close second, but sertraline remains the gold standard.
Can I get help if I don’t have insurance or am on Medicaid?
Yes. As of 2023, 87% of Medicaid programs require documented OB/GYN-psychiatrist coordination for reimbursement, meaning these services are covered. Many academic hospitals offer free or low-cost perinatal mental health clinics. Project TEACH NY and similar programs provide telehealth consultations with specialists at no cost to the patient. Call your local health department or search for “perinatal mental health program” + your state. You’re entitled to care-don’t let insurance myths stop you.





Write a comment
Your email address will be restricted to us