Why pediatric diabetes needs a fresh look
Diabetes in kids isn’t just "adult‑type" disease hidden in a younger body. Over the past decade, more children are being diagnosed with type 2 diabetes, driven by rising obesity rates and sedentary lifestyles. Parents and clinicians often struggle with the question: can we safely use the same medicines we give adults, or do kids need a customized approach?
The answer isn’t black‑and‑white, but a growing body of research suggests that some adult‑approved drugs, when dosed carefully, can fill gaps left by lifestyle changes and older meds. That’s where saxagliptin enters the conversation.
What is saxagliptin?
Saxagliptin is a DPP‑4 inhibitor that helps lower blood glucose by prolonging the action of incretin hormones, which boost insulin release after meals and reduce glucagon production. It was first approved by the FDA in 2009 for adults with type 2 diabetes. Since then, clinicians have explored off‑label use in adolescents because the drug’s oral route and once‑daily dosing fit well with a teen’s busy schedule.
Understanding pediatric type 2 diabetes
When we say “pediatric diabetes,” most readers think of type 1, but the focus here is Type 2 Diabetes in children. Unlike the autoimmune attack in type 1, type 2 stems from insulin resistance, often linked to excess weight, poor diet, and limited physical activity. The disease presents with higher fasting glucose, elevated HbA1c levels, and sometimes early signs of metabolic syndrome.
Guidelines from the American Diabetes Association advise lifestyle intervention as the first line, but many families need medication to reach target glucose levels within weeks, not months.
How saxagliptin works in children
The core mechanism of saxagliptin doesn’t change between adults and kids: it blocks the enzyme dipeptidyl peptidase‑4 (DPP‑4). By doing so, it keeps incretin hormones like GLP‑1 active for longer, which prompts the pancreas to release more insulin after meals and tells the liver to cut back on glucose output.
Why is that useful for teens? Their hormonal spikes during puberty can make insulin response erratic. Saxagliptin’s steady boost helps smooth out post‑prandial spikes without the risk of hypoglycemia that insulin or sulfonylureas sometimes carry.

Clinical evidence and pediatric trials
Real‑world data is still catching up, but several Pediatric Clinical Trials have provided promising signals. A 2023 multicenter study enrolled 112 adolescents aged 12‑17 with HbA1c between 7.5% and 9.5%. Participants received saxagliptin 2.5 mg daily plus standard diet advice for 24 weeks.
- Mean HbA1c dropped 0.9 percentage points, comparable to metformin‑only groups.
- Only 4% reported mild gastrointestinal upset; no severe hypoglycemia was recorded.
- Adherence was 92% thanks to the pill’s once‑daily schedule.
Another small open‑label trial in New Zealand showed similar outcomes, with participants also experiencing modest weight stabilization, an important benefit given the obesity link.
Safety profile - what parents should watch for
Safety is the top concern for any pediatric medication. Saxagliptin’s side‑effect catalog includes:
- Upper respiratory infections (usually mild)
- Headache
- Rare cases of pancreatitis (monitor serum amylase/lipase if abdominal pain occurs)
The drug does not typically cause low blood sugar on its own, which makes it a safer partner when combined with metformin or lifestyle changes. However, the FDA has issued a warning about potential heart‑failure risk in older adults; that risk appears minimal in the adolescent population, but clinicians still screen for cardiac symptoms.
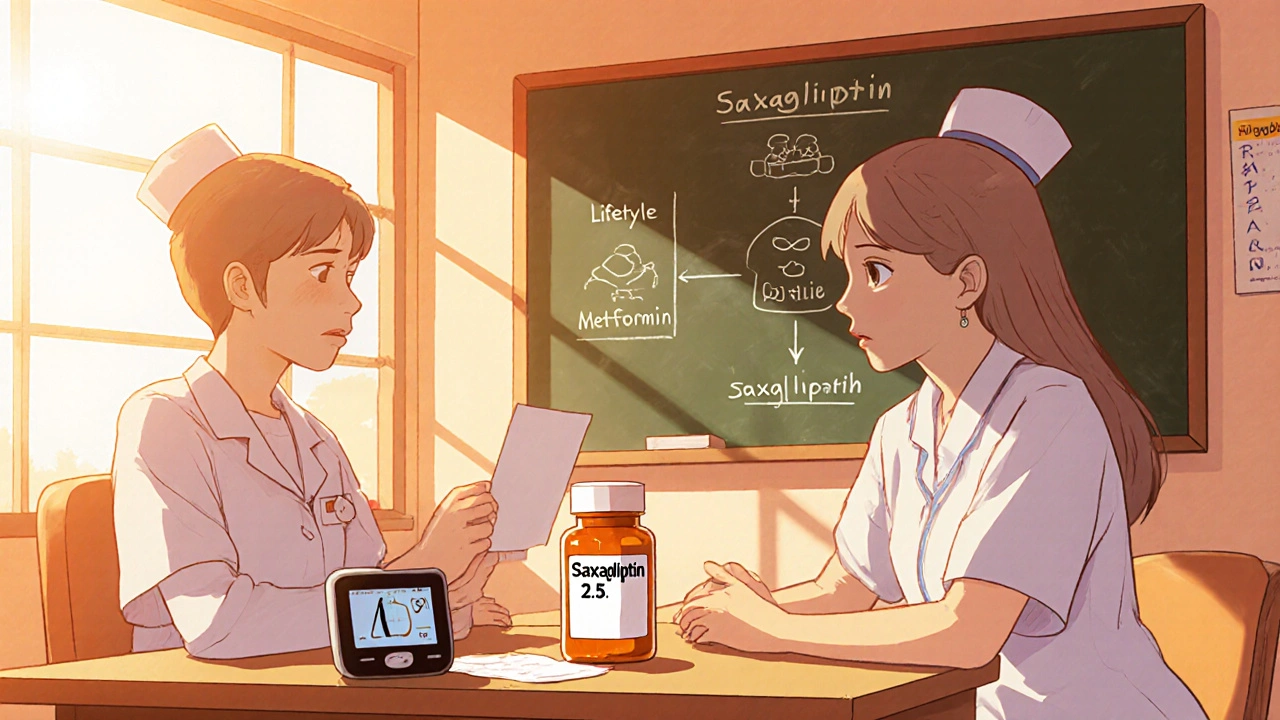
Building a saxagliptin‑based treatment plan
Step‑by‑step, here’s how a clinician might introduce saxagliptin into a teen’s regimen:
- Confirm diagnosis of type 2 diabetes via fasting glucose, HbA1c, and family history.
- Start with intensive Lifestyle Intervention: nutrition counseling, 60 minutes of moderate activity daily, and structured Glucose Monitoring at least twice a day. \n
- If HbA1c remains >7.0% after 8‑12 weeks, add metformin 500 mg once daily (titrated as tolerated).
- When metformin alone isn’t enough or causes GI upset, introduce saxagliptin 2.5 mg daily. Adjust to 5 mg only if weight and renal function allow.
- Schedule follow‑up labs at 3, 6, and 12 months: HbA1c, renal panel, and lipase if abdominal symptoms appear.
- Educate the teen on recognizing signs of pancreatitis (severe abdominal pain, vomiting) and when to call the clinic.
Throughout, involve parents in the education loop but empower the teen to manage their own medication kit - that autonomy improves adherence.
Comparing saxagliptin with other pediatric options
| Medication | Mechanism | Typical Dose (adolescents) | Age Approval | Common Side Effects |
|---|---|---|---|---|
| Saxagliptin | DPP‑4 inhibition (increases incretin action) | 2.5 mg - 5 mg daily | Off‑label; studied 12‑17 y | Headache, URIs, rare pancreatitis |
| Metformin | Biguanide (reduces hepatic glucose output) | 500 mg - 1000 mg BID | Approved ≥10 y | GI upset, vitamin B12 deficiency |
| Insulin (basal‑bolus) | Direct glucose uptake | Weight‑based dosing (0.2‑0.5 U/kg) | Approved all ages | Hypoglycemia, weight gain |
When you stack the table, a few takeaways pop up:
- Saxagliptin offers a middle ground - oral, once‑daily, low hypoglycemia risk.
- Metformin remains the first‑line drug because of its long safety record, but GI side effects can push families toward alternatives.
- Insulin is still the gold standard for severe hyperglycemia, yet the injection burden often reduces teen compliance.
Practical tips and common pitfalls
Even the best drug can fail without smart implementation. Here are nuggets of advice gathered from pediatric endocrinology clinics:
- Never mix up dosing units. Saxagliptin comes in 2.5 mg tablets; misreading a 5 mg dose as 50 mg can happen if the pill bottle isn’t clearly labeled.
- Pair saxagliptin with a structured Glucose Monitoring plan. A single “high” reading without context will lead to unnecessary dose changes.
- Watch kidney function. The drug is excreted renally, so a creatinine clearance < 60 mL/min requires dose reduction or avoidance.
- Engage school nurses. Many teens forget doses during exam weeks; a simple note in the school health record helps keep the routine intact.
- Avoid abrupt discontinuation. If side‑effects arise, taper over 1‑2 weeks rather than stopping cold‑turkey, to prevent rebound hyperglycemia.
Frequently Asked Questions
Is saxagliptin approved for kids?
No. The FDA has only approved saxagliptin for adults. However, pediatric endocrinologists often prescribe it off‑label after weighing benefits against risks, especially for adolescents who cannot tolerate metformin.
How quickly can I expect blood‑sugar improvement?
Most teens see a 0.5‑0.9 % drop in HbA1c after 12‑16 weeks of consistent dosing, provided diet and activity remain stable.
Can saxagliptin be combined with insulin?
Yes, it’s often added to basal insulin to reduce post‑meal spikes without increasing hypoglycemia risk. Dose adjustments are needed and should be overseen by a specialist.
What should I do if my child feels nauseous?
Nausea is more common with metformin than saxagliptin. If it occurs, check timing (maybe the drug is taken on an empty stomach) and consider taking it with food. Persistent symptoms warrant a call to the clinic.
Are there any long‑term concerns?
Long‑term data in teens are limited, but adult registries show no major safety signals beyond rare pancreatitis. Ongoing monitoring of liver and kidney function is recommended.
Bottom line: saxagliptin isn’t a magic bullet, but for the right adolescent-one who needs an oral option, can’t tolerate metformin, and has good renal function-it can be a valuable piece of the puzzle.


Write a comment
Your email address will be restricted to us