When a child snores loudly, stops breathing during sleep, or wakes up gasping for air, it’s not just a noisy night-it could be pediatric sleep apnea. This isn’t rare. About 1 to 5 out of every 100 children have it, and most cases happen between ages 2 and 6, when their tonsils and adenoids are biggest compared to their airways. These soft tissues, meant to protect against infection, can grow too large and block the throat while they sleep. The result? Repeated pauses in breathing, low oxygen levels, and broken sleep that affects everything from school performance to heart health.
Why Tonsils and Adenoids Are the Main Culprit
Most kids with sleep apnea don’t have it because of weight, allergies, or jaw structure. It’s because their tonsils and adenoids are swollen. These are lymphoid tissues at the back of the throat and nose. In childhood, they naturally grow larger as the immune system develops. But in some kids, they grow too much-blocking the airway like a cork in a bottle.
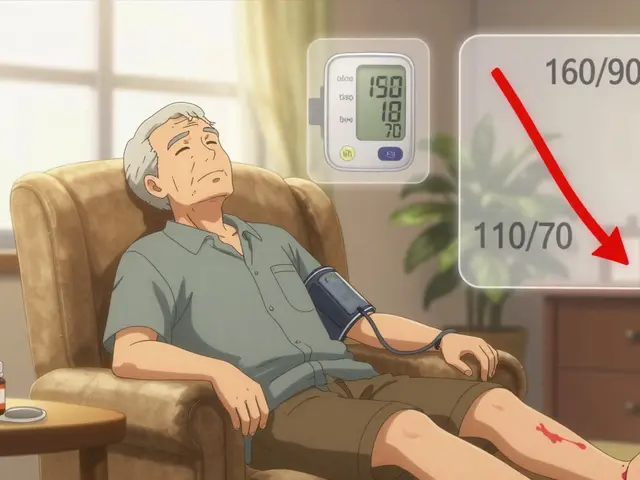
Doctors call this obstructive sleep apnea (OSA). During sleep, muscles relax, and when the airway is already narrow, the tissue collapses inward. Breathing stops for 10 seconds or more, sometimes dozens of times an hour. The brain wakes the child up just enough to take a breath, but not enough for real rest. Over time, this leads to daytime fatigue, trouble concentrating, behavioral issues, and even high blood pressure.
Studies from the American Thoracic Society show that children with severe OSA can have 15 to 30 breathing pauses every hour. That’s like being woken up 20 times a night without ever realizing it. No wonder they act out in class or fall asleep in the car.
The Gold Standard: Adenotonsillectomy
The first-line treatment? Remove the blockage. That means surgery-adenotonsillectomy-which is the removal of both the adenoids (behind the nose) and the tonsils (at the back of the throat). It’s not a new idea. Since the 1980s, experts like Dr. Christian Guilleminault have linked these tissues directly to sleep apnea in kids.
Success rates? Between 70% and 80% in otherwise healthy children with enlarged tonsils and adenoids as the only issue. That’s why the American Academy of Pediatrics recommends this surgery as the first step. It’s not just about stopping snoring-it’s about protecting brain development, growth, and heart function.
But not all surgeries are the same. Traditional complete removal means more pain and a longer recovery-7 to 14 days on soft foods. Now, some centers like Yale Medicine offer partial tonsillectomy, where only part of the tonsil is taken out. This cuts recovery time by about 30% and reduces bleeding risk by half. It’s not everywhere yet, but it’s gaining traction.
Important note: both tissues need to go. Even if one looks bigger, removing just the tonsils or just the adenoids often leads to recurrence. Dr. David Gozal’s research shows that leaving even a small piece behind can let the apnea come back.
When Surgery Isn’t an Option: CPAP for Children
Not every child is a candidate for surgery. Some have neuromuscular disorders like cerebral palsy. Others have craniofacial abnormalities, severe obesity, or bleeding risks. For them, CPAP (Continuous Positive Airway Pressure) is the go-to solution.
CPAP works by gently pushing air through a mask worn during sleep. The pressure keeps the airway open-like holding a straw open with your fingers. For kids, the pressure is usually set between 5 and 12 cm H2O, carefully adjusted during a sleep study to find the sweet spot: enough to stop apneas, but not so much it feels suffocating.
When used correctly, CPAP is 85% to 95% effective. That’s even better than surgery for kids with obesity-related OSA, where surgery success drops to under 50%. It’s also the top choice for children who still have apnea after surgery.
But here’s the catch: kids hate the mask. At Children’s National Hospital, 30% to 50% of kids stop using CPAP because it’s uncomfortable, scary, or they feel trapped. That’s why fitting matters. Pediatric masks come in different shapes-nasal pillows, full face, or nasal prongs. A good sleep specialist will try several until the child finds one that doesn’t feel like a space helmet.
Parents need patience. It can take weeks to months for a child to adjust. Some need bedtime routines that include wearing the mask while watching TV, then gradually adding it during sleep. Refitting every 6 to 12 months is also key-kids grow fast, and a mask that fit last year won’t work this year.

Other Treatments: What Else Works?
Not every child needs surgery or CPAP. For mild cases, doctors sometimes start with less invasive options.
- Inhaled corticosteroids-like fluticasone-can shrink swollen adenoids. A daily spray (88-440 mcg) may help, especially if allergies are involved. But it takes 3 to 6 months to see results, and it’s not a cure.
- Montelukast (a leukotriene blocker) is used for kids with allergy-related swelling. It’s not FDA-approved for sleep apnea, but studies show it helps reduce symptoms in about 30-50% of mild cases.
- Rapid maxillary expansion-an orthodontic device that widens the upper jaw-works well in kids with narrow palates. It’s slow (6-12 months), but can improve airflow by 60-70% in the right candidates.
These are not replacements for surgery or CPAP in moderate to severe cases. But for mild OSA, they’re worth trying-especially if parents want to avoid procedures.
What Happens After Treatment?
Even after surgery or starting CPAP, the work isn’t done. Follow-up sleep studies are critical. The American Thoracic Society says kids with severe OSA should have another sleep study 2 to 3 months after surgery to make sure the apnea is truly gone.
Some kids improve but don’t fully recover. Others develop new problems-like central sleep apnea, where the brain stops sending the signal to breathe. That’s when CPAP settings need adjusting. Cleveland Clinic experts say most issues like this can be fixed with a pressure tweak in 1 to 2 weeks.
And yes, apnea can come back. If a child gains weight, gets sick with a bad cold, or develops new nasal congestion, the airway can close again. That’s why ongoing monitoring matters.

What Parents Should Watch For
Here are signs your child might have sleep apnea:
- Loud, regular snoring (not just occasional)
- Gasping, choking, or snorting during sleep
- Mouth breathing while awake or asleep
- Restless sleep-tossing and turning all night
- Daytime sleepiness, irritability, or trouble paying attention
- Bedwetting that started after age 5
- Growth delays or poor weight gain
If you notice two or more of these, talk to your pediatrician. They may refer you to a pediatric sleep specialist for a sleep study.
What’s New in the Field
Science is moving fast. In 2022, the FDA approved a new device called hypoglossal nerve stimulation for select children with severe OSA. It’s a small implant that gently stimulates the tongue to keep it from blocking the airway. It’s still rare and expensive, but it’s an option for kids who can’t use CPAP and aren’t surgical candidates.
Another emerging tool is drug-induced sleep endoscopy (DISE). Instead of a full sleep study, a doctor uses mild sedation to watch the airway collapse in real time during sleep. This helps surgeons plan exactly which tissues to remove, making operations more precise.
Researchers are also testing high-dose nasal steroids to shrink tonsils without surgery. Early trials show a 20-30% reduction in tissue size after 6 months. Still experimental, but promising.
Despite all the new tech, adenotonsillectomy remains the most common treatment. About 85-90% of kids with OSA start here. CPAP use is growing too-up 5-7% each year-as doctors realize it’s not just for adults.
Final Thoughts
Pediatric sleep apnea isn’t something you just grow out of. Left untreated, it can affect a child’s brain, heart, and future. But the good news? We have effective tools.
For most healthy kids with big tonsils and adenoids, surgery is the fastest path to a full recovery. For others-with complex medical issues or after surgery fails-CPAP works wonders. And for mild cases, medications or orthodontics might be enough.
The key is not to wait. If your child snores loudly, breathes through their mouth, or seems tired all day, get it checked. A simple sleep study can change their life.






Write a comment
Your email address will be restricted to us