Why Your Plate Matters More Than You Think
If you’ve been told you have prediabetes, you’re not alone-nearly 1 in 3 adults in the U.S. have it, and most don’t even know. But here’s the good news: you can stop it from turning into type 2 diabetes. Not with pills. Not with magic supplements. But with what you eat. The science is clear. Changing how you eat can slash your risk by more than half. And it all comes down to three simple things: fiber, protein, and the glycemic index of your food.
You don’t need to become a nutritionist. You don’t need to count every calorie. You just need to make smarter choices, one meal at a time. Think less about cutting out food and more about adding in what actually helps your body stay balanced.
Fiber: Your Body’s Natural Blood Sugar Shield
Fiber doesn’t get digested. That’s why it’s so powerful. Instead of turning into sugar like other carbs, it moves through your system slowly, pulling glucose along with it. This keeps your blood sugar from spiking after meals.
The goal? 25 to 38 grams a day. That’s not as hard as it sounds. One cup of cooked lentils gives you 15 grams. A medium apple with skin? 4.5 grams. Half a cup of broccoli? 2.5 grams. A slice of whole grain bread? 3 grams.
Most people eat less than half of what they need. Start by making half your plate non-starchy vegetables-spinach, peppers, zucchini, cauliflower. These are low in carbs, high in fiber, and won’t spike your blood sugar. Swap white rice for barley or quinoa. Choose steel-cut oats over instant. They take longer to digest, so your blood sugar rises slowly instead of crashing later.
A 2021 study found that every extra 10 grams of fiber you eat daily cuts your diabetes risk by 23%. That’s like getting a free insurance policy for your pancreas.
Protein: The Silent Stabilizer
Protein doesn’t raise blood sugar much at all. But here’s the trick-it slows down how fast carbs turn into sugar. That’s why pairing fruit with nuts, or yogurt with berries, works so well.
Instead of grabbing a banana alone, have it with a tablespoon of almond butter. Eat an apple with a hard-boiled egg. Have Greek yogurt with chia seeds. These combos keep your glucose under control for hours.
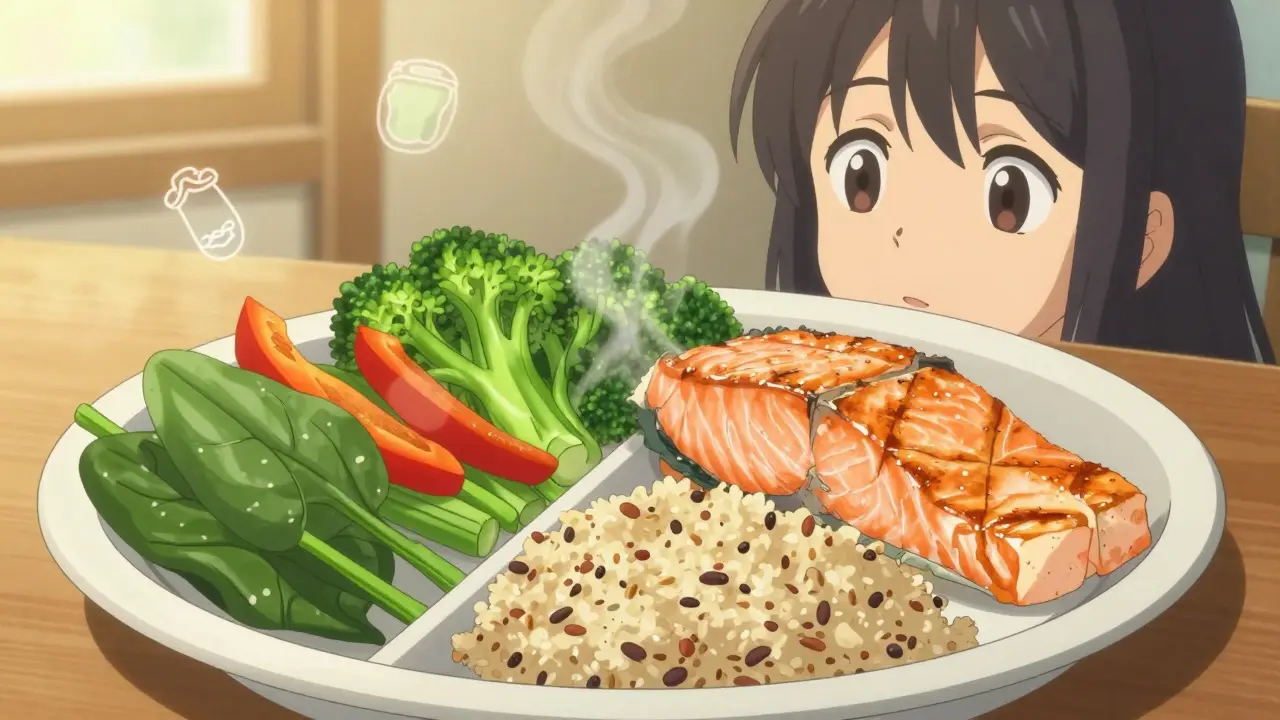
Focus on lean sources: fish, chicken, turkey, eggs, tofu, lentils, beans. Skip the processed meats-bacon, sausage, deli slices. They’re loaded with sodium and preservatives that make insulin work harder.
Red meat? Limit it. A 2020 study showed that eating just 100 grams of red meat a day-about the size of a deck of cards-raises your diabetes risk by 20%. That’s not because of the fat. It’s because of the iron and compounds that build up in muscle tissue over time.
Plant proteins like beans and lentils are double wins. They give you protein AND fiber. A bowl of black bean soup? You’re hitting two targets at once.

Glycemic Index: Not All Carbs Are Created Equal
Carbs aren’t the enemy. But some carbs turn into sugar faster than others. That’s what the glycemic index (GI) measures. High-GI foods cause quick spikes. Low-GI foods give you steady energy.
Here’s what to avoid:
- White bread (GI 75)
- White rice (GI 73)
- Potatoes (GI 85)
- Sugary cereals (GI 80+)
- Regular soda and fruit juice
Here’s what to choose instead:
- Quinoa (GI 53)
- Sweet potatoes (GI 44)
- Oats (GI 55)
- Barley (GI 28)
- Legumes like chickpeas and lentils (GI 28-32)
- Most fruits: berries, apples, pears, kiwi
A 2022 study showed that people who stuck to a low-GI diet (average GI of 45) lowered their HbA1c by 0.5% in just six months. That’s the same drop you’d see with some diabetes medications-but without side effects.
Don’t obsess over the exact number. Just remember: the more processed, the higher the GI. The more whole, the lower.
The Mediterranean Diet: The Gold Standard
Doctors don’t just recommend the Mediterranean diet because it’s trendy. They recommend it because it works. It’s not a diet. It’s a way of eating that’s been studied for decades.
What’s on the plate? Lots of vegetables, olive oil, fish, nuts, beans, whole grains, and fruit. Small amounts of dairy and poultry. Rarely red meat. No processed snacks or sugary drinks.
Research shows it improves blood sugar control, lowers bad cholesterol, and reduces heart disease risk-all things people with prediabetes need to worry about. The American Diabetes Association calls it one of the best eating patterns for prediabetes.
You don’t need to eat Greek food every night. Just start with one change: swap butter for olive oil. Replace white pasta with whole grain. Add a handful of walnuts to your salad. These small shifts add up.
Real People, Real Results
One person on a diabetes forum switched from instant oatmeal to steel-cut oats. Their morning blood sugar dropped by 30 points-consistently. Another swapped a bagel for whole grain toast with avocado and eggs. Their post-meal glucose stayed under 140 instead of spiking to 180.
But here’s the hard part: most people quit. A survey found that 42% struggled to eat enough veggies every day. Another 68% had trouble with portion control.
Here’s a trick that works: use your plate as a guide.
- Half the plate: non-starchy vegetables
- One-quarter: lean protein
- One-quarter: whole grains or starchy vegetables
That’s it. No measuring cups. No apps. Just a visual cue your brain understands.
What to Avoid (For Real)
Some foods are obvious enemies: candy, soda, pastries. But others sneak in.
- Flavored yogurt-often has more sugar than ice cream
- Granola bars-loaded with honey and dried fruit
- “Healthy” juices-even 100% fruit juice spikes blood sugar fast
- Margarine and hard cooking fats-high in trans fats that worsen insulin resistance
- White flour products-even if labeled “enriched,” they act like sugar
Read labels. Look for added sugars. If sugar is in the first three ingredients, put it back.
Limit added sugars to less than 10% of your daily calories. That’s about 50 grams-or 12 teaspoons-for most people. One can of soda has 39 grams.
Small Steps, Big Changes
You don’t have to overhaul your life tomorrow. Start with one meal. Maybe breakfast. Swap sugary cereal for oatmeal with berries and almonds. That’s one win.
Next week, swap white rice for quinoa at dinner. Add a side of steamed broccoli. Another win.
After a month, you’ve made three changes that add up to a new habit. And habits are what keep you from getting diabetes.
The goal isn’t perfection. It’s progress. The Diabetes Prevention Program proved that losing just 5% of your body weight cuts diabetes risk by 58%. That’s 10 pounds for someone who weighs 200. You don’t need to lose 50. Just 10.
And you don’t need to do it alone. Programs like the National Diabetes Prevention Program (covered by Medicare) offer coaching, group support, and tools. If you’re in the U.S., check if you qualify. If you’re elsewhere, look for local health services offering lifestyle programs.
It’s Not About Deprivation. It’s About Power.
Prediabetes isn’t a life sentence. It’s a warning sign-and you have the power to change it. Fiber slows the rush of sugar. Protein keeps you full and steady. Low-GI foods give you energy without the crash.
This isn’t about eating bland food. It’s about eating food that works with your body, not against it. It’s about feeling better, having more energy, and not worrying about your next blood test.
Start today. Not tomorrow. Not Monday. Today. Pick one thing: add a veggie to your lunch. Swap one carb for a whole grain. Have a handful of nuts instead of crackers.
Your future self will thank you.






Write a comment
Your email address will be restricted to us