When someone vomits blood or passes black, tarry stools, it’s not just unpleasant-it’s a medical emergency. Upper GI bleeding can turn deadly in hours if not handled right. It’s not rare: about 100 people out of every 100,000 experience it each year in the U.S., and the numbers are rising as the population ages. The real danger? Many people ignore early signs, thinking it’s just indigestion or a bad meal. But when bleeding comes from the esophagus, stomach, or first part of the small intestine, every minute counts.
What Causes Upper GI Bleeding?
The most common culprit is peptic ulcer disease, responsible for nearly half of all cases. These are open sores in the stomach lining or duodenum, often caused by H. pylori bacteria or long-term use of NSAIDs like ibuprofen or aspirin. Gastric ulcers make up 20-30% of these cases, while duodenal ulcers are more frequent, accounting for 70-80%. What’s alarming is that many patients have no warning symptoms until they start bleeding. Another major cause is esophageal varices-swollen, fragile veins in the lower esophagus. These develop in people with advanced liver disease, especially cirrhosis. Portal hypertension forces blood to find new paths, and these veins balloon under pressure. When they rupture, the bleeding is sudden and massive. About 1 in 5 upper GI bleeds comes from varices, and the 6-week mortality rate is around 20%. Other causes include:- Erosive gastritis (15-20%)-inflammation that wears away the stomach lining
- Esophagitis (5-10%)-often from acid reflux or infections
- Mallory-Weiss tears (5-10%)-rips at the junction of the esophagus and stomach, usually after violent vomiting
- Malignancies (2-5%)-stomach or esophageal cancer
- Hiatal hernias (about 5%)-where part of the stomach pushes into the chest, sometimes causing irritation
Even medications can trigger bleeding. A 2022 JAMA study found that people taking SSRIs (common antidepressants) had double the risk of upper GI bleeding compared to those who didn’t. And if you’re on blood thinners or NSAIDs? Your risk goes up even more.
Recognizing the Signs
The body doesn’t lie. If you’re bleeding from the upper GI tract, your symptoms are unmistakable:- Hematemesis-vomiting bright red blood, or material that looks like coffee grounds. That dark, gritty appearance means the blood has been partially digested.
- Melena-black, sticky, foul-smelling stools. This is digested blood passing through the intestines.
- Hematochezia-bright red or maroon stools. This usually means massive bleeding, where blood moves too fast to be digested.
- Dizziness, fainting, rapid heartbeat-signs your body is struggling to keep up with blood loss.
- Low blood pressure-systolic pressure below 90 mmHg is a red flag.
Some patients don’t feel pain at all. Others report a dull ache or burning. The absence of pain doesn’t mean it’s not serious. In fact, many people with variceal bleeding feel nothing until they collapse.
A 2023 Reddit post from a user named u/GIwarrior99 described waking up at 3 a.m. coughing up coffee-ground material. He went to the ER, got three units of blood, and spent eight days in the hospital. His story isn’t unusual. What is unusual? People who wait. One user, u/StomachSOS, had black stools dismissed as “iron supplements” for two weeks-until their hemoglobin dropped to 5.8 g/dL (normal is 12-16). They collapsed. That’s the kind of delay that kills.
Stabilization: The First 30 Minutes
Before you even think about endoscopy or surgery, you stabilize. That means protecting the airway, restoring blood volume, and preventing shock.- Put the patient in a supine position with legs elevated.
- Start two large-bore IV lines immediately.
- Check vital signs: heart rate over 100, systolic BP under 90? That’s a high-risk patient.
- Draw blood for CBC, INR, BUN, creatinine, and type & crossmatch.
The BUN-to-creatinine ratio is a hidden clue. If it’s above 30:1, there’s a 69% chance the bleeding is upper GI-not lower. It’s not perfect, but it’s fast and free.
Transfusion isn’t always needed. The goal isn’t to get hemoglobin back to normal. It’s to keep it between 7 and 9 g/dL. Giving too much blood too fast can cause fluid overload, especially in patients with heart or liver disease. Each unit of packed red blood cells raises hemoglobin by about 1 g/dL.
For variceal bleeding, antibiotics are critical. Ceftriaxone 1g IV daily reduces infection-related deaths by 30%. Why? Because liver disease weakens the immune system, and bleeding creates a perfect storm for bacteria to invade the gut.
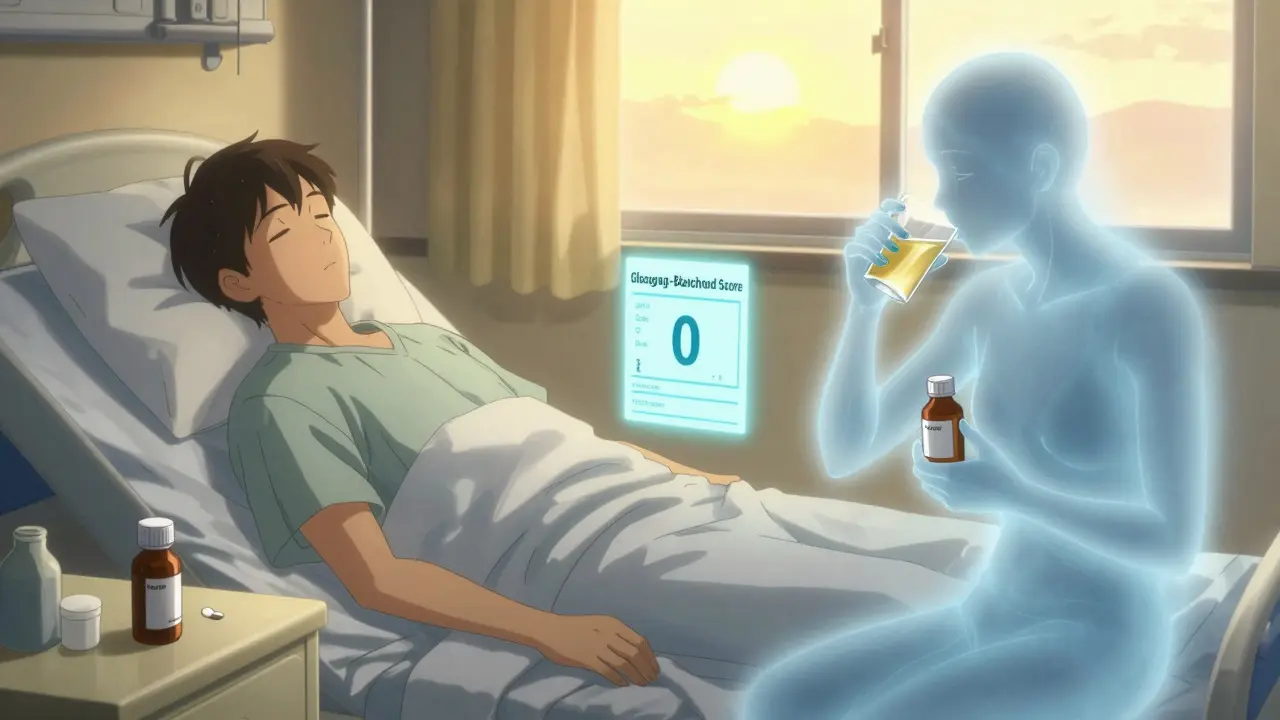
The Glasgow-Blatchford Score: Your Triage Tool
Not every patient needs to be rushed to endoscopy. That’s where the Glasgow-Blatchford score comes in. Developed in 2000 and updated in 2019, it uses six simple, objective numbers:- Hemoglobin level (less than 12.9 for men, less than 11.9 for women)
- Systolic blood pressure (under 100 mmHg)
- Pulse rate (over 100 bpm)
- Melena
- History of syncope (fainting)
- History of liver disease or heart failure
Add them up. A score of 2 or higher means hospitalization is needed. A score of 0? You might be able to send them home safely. A 2023 study showed that 15% of upper GI bleed patients can be managed as outpatients-saving beds, money, and stress.
Doctors who skip this step often over-treat. One study found 30% of low-risk patients got unnecessary PPIs and endoscopies because they didn’t use the score. That’s waste-and risk.
Endoscopy: The Gold Standard
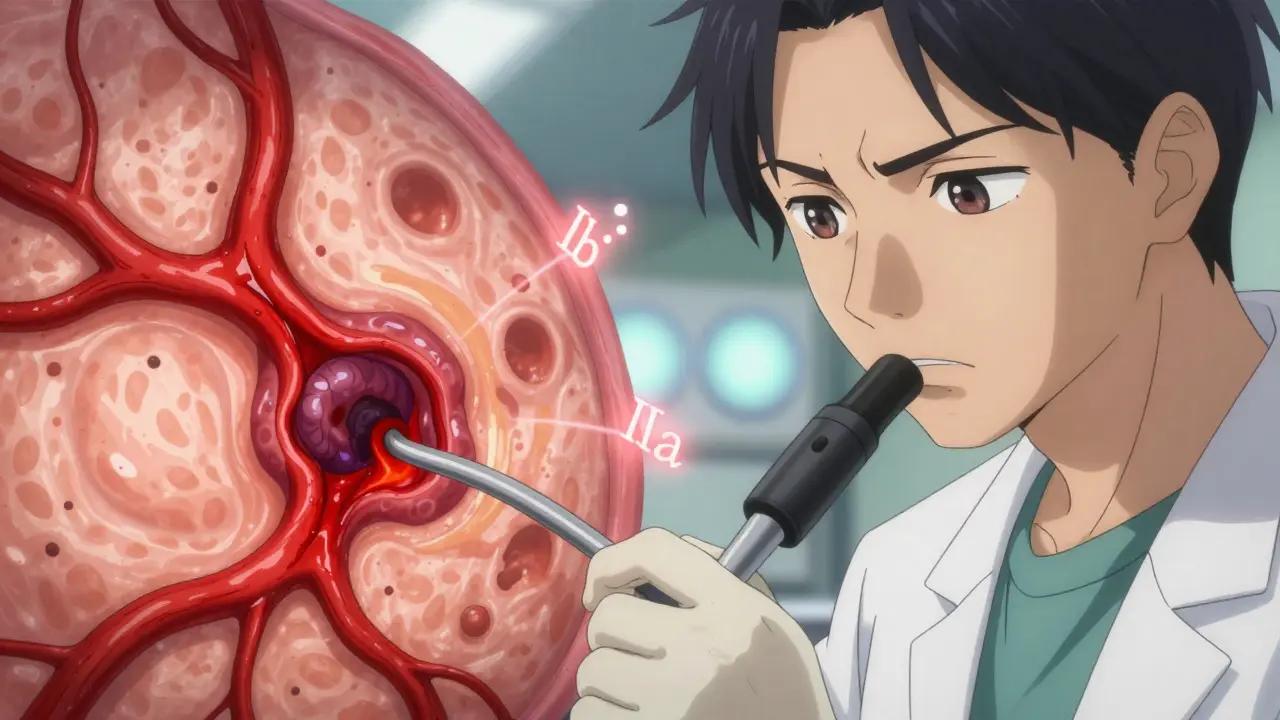
Time is tissue. The American College of Gastroenterology recommends endoscopy within 24 hours. But here’s the kicker: if you do it within 12 hours, mortality drops by 25% for high-risk patients.During the procedure, doctors use the Forrest classification to assess bleeding risk:
- Class Ia-spurting blood. 90% chance of rebleeding without intervention.
- Class Ib-oozing. 50% rebleeding risk.
- Class IIa-visible vessel. Also 50% risk.
- Class IIb-adherent clot. 20% risk.
- Class III-clean base. Less than 5% risk.
For non-variceal bleeding (like ulcers), the standard treatment is a combo of:
- 80mg IV pantoprazole bolus, then 8mg/hour infusion
- Epinephrine injection to constrict blood vessels
- Hemoclips or thermal coagulation to seal the site
This approach stops bleeding in 90-95% of cases. The COBALT trial showed PPIs alone cut rebleeding from 22.6% to 11.6%.
For varices, band ligation is preferred. It reduces rebleeding from 60% to 25%. Sclerotherapy? Outdated. Vasoactive drugs like terlipressin or octreotide are given immediately to lower portal pressure. Combine that with antibiotics, and you cut mortality by 25%.
What’s New in 2026?
Technology is changing the game. In 2023, the FDA approved Hemospray, a powder that forms a physical barrier over bleeding spots. It’s not a cure, but it’s a lifesaver when the source is hard to reach or the patient is too unstable for standard endoscopy.Even bigger? AI-assisted endoscopy. A 2023 trial showed AI systems spotted subtle bleeding signs with 94.7% accuracy-far better than human eyes at 78.3%. But here’s the catch: these systems were trained mostly on data from white patients. In Black and Hispanic patients, accuracy drops by 15%. That’s not just a technical flaw-it’s a health equity issue.
The NIH’s UGIB-360 study, launched in January 2024, is tracking 10,000 patients to build personalized risk models using genetics, gut bacteria, and clinical history. Results won’t be ready until late 2025, but the goal is clear: predict who’s at risk before they bleed.
What Happens After?
Recovery isn’t just about stopping the bleed. It’s about preventing the next one.- Test for H. pylori. If positive, treat with antibiotics and a PPI.
- Stop NSAIDs. Switch to acetaminophen if possible.
- For varices, consider beta-blockers like propranolol to lower portal pressure long-term.
- Follow up with a gastroenterologist within 72 hours.
Patients often don’t realize how much they’ve changed. A 2022 study found 68% were anxious about bleeding again. 42% quit spicy food, caffeine, and alcohol. 31% stopped NSAIDs on their own-without telling their doctor. That’s dangerous. You need guidance, not guesswork.
Hospitals that use the “Upper GI Bleed Bundle”-rapid assessment, risk scoring, PPI within an hour, endoscopy within 12 hours, follow-up within 72 hours-cut their 30-day mortality from 8.7% to 5.3%. That’s not magic. It’s protocol.
Final Thoughts
Upper GI bleeding isn’t a diagnosis you make from a textbook. It’s a clinical emergency that demands speed, precision, and teamwork. Whether it’s a bleeding ulcer from years of ibuprofen, or a ruptured varix from undiagnosed cirrhosis, the principles are the same: stabilize fast, assess smartly, treat early, and follow up.And if you’re a patient? Don’t wait. Don’t assume it’s heartburn. If you’re vomiting blood or passing black stools, go to the ER. Your life might depend on it.
What does coffee-ground vomit mean?
Coffee-ground vomit means blood has been in the stomach long enough to be partially digested by stomach acid. It’s a classic sign of upper GI bleeding, often from a peptic ulcer or gastritis. It’s not a minor issue-it requires urgent medical evaluation.
Can you have upper GI bleeding without pain?
Yes. Many people, especially older adults and those on blood thinners, bleed without any abdominal pain. Symptoms like dizziness, rapid heartbeat, or black stools may be the only warning signs. Pain is not a reliable indicator of severity.
Is upper GI bleeding life-threatening?
Absolutely. Up to 10% of patients die within 30 days of a major bleed, and mortality jumps to 20% with esophageal varices. Delayed treatment increases risk dramatically. Early intervention reduces death rates by 25% or more.
What’s the difference between melena and hematochezia?
Melena is black, sticky, tar-like stool caused by digested blood from the upper GI tract. Hematochezia is bright red or maroon blood in stool, usually indicating faster bleeding-either from a massive upper GI bleed or a lower GI source like the colon. Both need emergency care.
Do I need an endoscopy if I had one episode of black stool?
Yes. Even a single episode of melena suggests bleeding somewhere in the upper GI tract. Endoscopy is the only way to find the source and stop it. Skipping it risks rebleeding, which is more dangerous and harder to treat.
Can I take ibuprofen again after a GI bleed?
Not without your doctor’s approval. NSAIDs like ibuprofen are a leading cause of ulcers and rebleeding. If you need pain relief, acetaminophen is safer. If you must use NSAIDs long-term, your doctor may prescribe a PPI alongside it-but only after evaluating your risk.
How long does recovery take after an upper GI bleed?
Most people recover physically within 2-4 weeks if the bleed is controlled and the cause is treated. But emotional recovery takes longer-many feel anxious for months. Follow-up care, medication adherence, and lifestyle changes are critical to prevent recurrence.





Write a comment
Your email address will be restricted to us