What if you could hear again - not by putting a tiny speaker in your ear, but by feeling sound through your skull? That’s exactly what bone-conduction hearing aids do. They don’t amplify sound like regular hearing aids. Instead, they send vibrations straight through the bone behind your ear to your inner ear, skipping the outer and middle ear entirely. For people with chronic ear infections, congenital ear deformities, or single-sided deafness, this isn’t just a novelty - it’s often the only way to hear clearly.
How Bone-Conduction Hearing Aids Actually Work
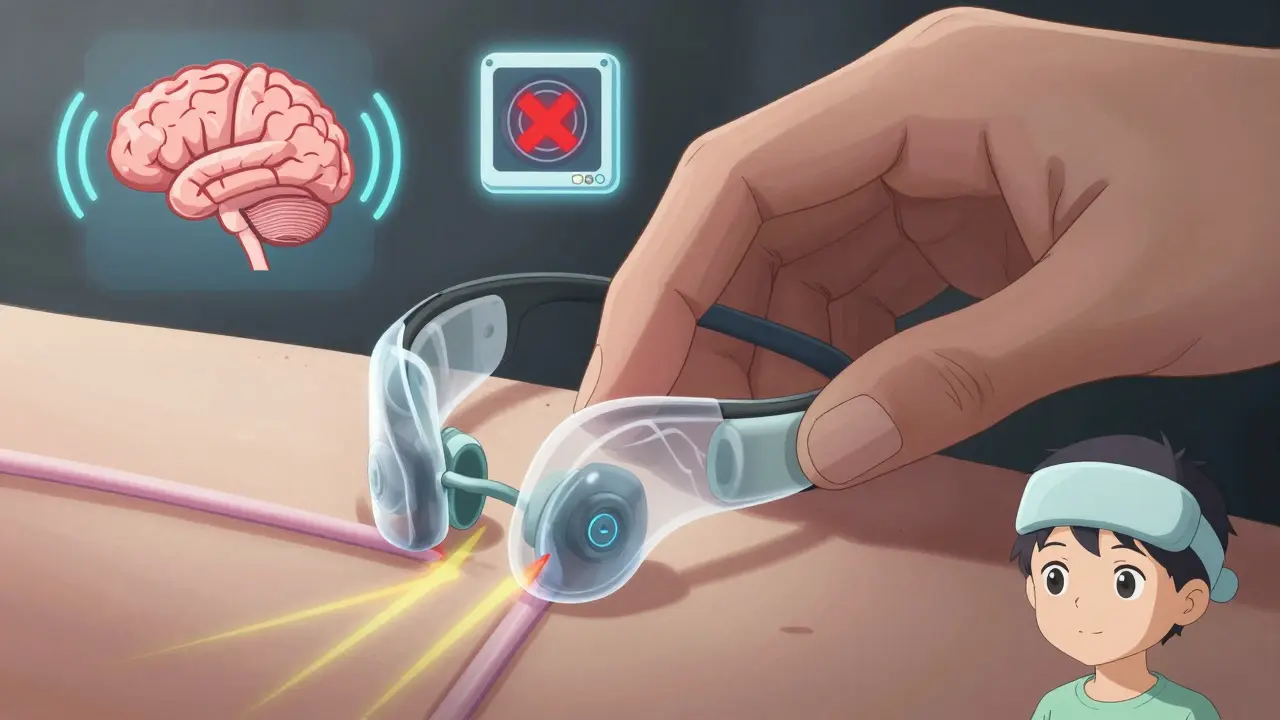
Normal hearing relies on sound waves traveling through the ear canal, vibrating the eardrum, and then moving tiny bones in the middle ear to stimulate the cochlea. But when any part of that chain is blocked - by wax, infection, or malformed anatomy - sound can’t get through. That’s where bone conduction comes in.
These devices use the skull’s natural ability to conduct sound. When a sound processor vibrates against the bone behind the ear, those vibrations travel through the skull and directly stimulate the cochlea. It’s the same principle that lets you hear your own voice when you speak - you’re not just hearing it through the air, you’re feeling it in your bones.
This method bypasses all the parts that might be damaged or blocked. It doesn’t matter if your ear canal is narrow, your eardrum is scarred, or you’ve lost hearing in one ear. As long as your inner ear (cochlea) still works, bone conduction can deliver sound. Studies show speech understanding improves by 20-35% in noisy environments for people with single-sided deafness using these devices.
Who Benefits Most From Bone-Conduction Hearing Aids?
Not everyone with hearing loss is a candidate. These devices are designed for three specific conditions:
- Conductive hearing loss: Sound can’t get through the outer or middle ear due to infection, fluid, or structural issues. This is common in people with chronic ear infections or children born with aural atresia (a missing or closed ear canal).
- Mixed hearing loss: A combination of conductive and sensorineural loss. Bone conduction helps by overcoming the conductive part.
- Single-sided deafness (SSD): When one ear is completely deaf but the other works fine. Traditional hearing aids can’t help here - but bone conduction lets the brain receive sound from the deaf side by sending vibrations across the skull to the good ear.
For people with chronic ear infections, traditional hearing aids are often impossible to use. The ear canal must stay dry and clean, but infections make that unmanageable. In these cases, bone conduction devices are medically necessary - and 92% of patients with recurrent infections can’t use regular hearing aids at all.
Children born with aural atresia have a 85-90% success rate with bone conduction implants. Many grow up never hearing properly - until they get one. Adults with sudden SSD after trauma or illness report life-changing results: hearing birds on their deaf side for the first time in years, understanding conversations in crowded rooms, and no longer feeling isolated.
Percutaneous vs. Transcutaneous: Two Different Approaches
There are two main types of bone-conduction systems: those that go through the skin and those that work through it.
Percutaneous systems (like Cochlear’s BAHA Connect and Oticon’s Ponto 5) involve a titanium implant surgically fused to the skull bone. After 3-6 months of healing, an abutment sticks out through the skin, and the sound processor snaps onto it. These deliver the strongest signal - up to 50 dB of gain - making them ideal for severe hearing loss.
But there’s a trade-off. About 15-30% of users develop skin reactions around the abutment. Daily cleaning with 70% isopropyl alcohol is required. In 8% of cases, revision surgery is needed. One Reddit user wrote, "I had to take mine off every night because the skin got so irritated. It was a constant chore."
Transcutaneous systems (like MED-EL’s Bonebridge and Cochlear’s BAHA Attract) use magnets. The implant sits under the skin, and the external processor holds on magnetically. No hole in the skin means no infection risk from an abutment. Skin complications drop to under 5%. The downside? The signal weakens slightly as it passes through skin and tissue - losing 10-15 dB of power. That makes them less ideal for profound hearing loss.
Still, patient satisfaction is higher with transcutaneous systems. A 2023 MED-EL survey found 92% of Bonebridge users liked that no one could see their device. For people who work in public-facing jobs or just want to avoid the stigma of visible hardware, this matters.

Cost, Surgery, and Recovery
Getting a bone-conduction device isn’t as simple as buying a hearing aid. It requires surgery.
The procedure takes 30-60 minutes under local anesthesia. Most people go home the same day. Recovery is quick: you can return to normal activities in 48 hours. But there’s a waiting period before the device works.
With percutaneous systems, you wait 3-4 months for the titanium implant to fuse with the bone. Only then can the processor be activated. Transcutaneous systems can be turned on right after surgery - the magnets work immediately.
Costs are high. Implantable systems range from $4,000 to $7,000 per ear. That’s two to three times more than premium air-conduction hearing aids ($1,500-$3,500). Insurance often covers it if you have a documented medical need - especially for conductive loss or SSD - but prior authorization is required.
Some users worry about MRI scans. Most implants are MRI-compatible up to 1.5 Tesla, but the external processor must be removed. For 3T scans, the internal magnet may need surgical removal. That’s a major drawback for people who need frequent imaging.
How They Compare to Other Solutions
For single-sided deafness, the main alternative used to be CROS hearing aids - one device on the deaf side that wirelessly sends sound to the good ear. But CROS devices feel unnatural. They don’t help with sound localization. You can’t tell where a car is coming from, or who’s speaking across the table.
Bone conduction fixes that. A 2022 study in the Journal of the American Academy of Audiology found bone conduction devices improved speech reception thresholds by 15-20 dB compared to CROS systems. Users reported hearing conversations from both sides, feeling more connected in group settings.
Compared to cochlear implants, bone conduction is far less invasive. Cochlear implants replace the cochlea’s function entirely - they’re for people with severe nerve damage. Bone conduction only works if the cochlea is still healthy. That’s why it’s not used for profound sensorineural loss beyond 45-55 dB.
Real User Experiences
On Reddit’s r/Hearing community, 78% of recent posts from bone-conduction users report life-changing results. One user, u/AudiologyNerd, wrote: "I’ve had SSD since I was 12. For 15 years, I missed half the world. My first day with the Ponto, I heard a robin outside my window - on the side I thought was dead. I cried for an hour."
Others praise the comfort. "No more earwax buildup, no itching, no pressure in my ear canal," said a user with chronic otitis media. "I forget I’m wearing it."
But complaints exist. Skin irritation around the abutment is the top issue. MRI limitations frustrate many. And while transcutaneous systems avoid skin problems, they can slip off during intense exercise or when wearing headphones.
The Future of Bone-Conduction Technology
The market is shifting fast. In 2019, only 41% of new implants were transcutaneous. By 2023, that number jumped to 63%. Why? Fewer complications, better aesthetics, and improved magnet strength.
New devices are smarter. Cochlear’s BAHA 6 Max (2023) has Bluetooth 5.3, 30-hour battery life, and direct streaming from phones. MED-EL’s upcoming Bonebridge 3, launching in early 2024, uses AI to adjust sound based on environment - reducing background noise automatically.
The biggest leap? Fully implantable systems. Sonova is testing a device with no external parts - everything hidden under the skin, powered wirelessly. Phase III trials are complete, and FDA submission is expected by the end of 2024. If approved, this could eliminate the need for any visible hardware - and make bone conduction feel like natural hearing.
The market, now 5.2% of the global hearing aid industry, is growing at 8.7% annually - nearly double the rate of traditional hearing aids. By 2027, it’s expected to hit $1.1 billion. As awareness grows - especially around single-sided deafness - more people will realize they don’t have to live with half the world silenced.
What to Do Next
If you or someone you know has chronic ear infections, congenital ear issues, or single-sided deafness, talk to an audiologist who specializes in bone conduction. Not all clinics offer it. Ask for a referral to a center with experience in BAHA, Ponto, or Bonebridge systems.
Get a full hearing test. Confirm whether your cochlea is still functional - that’s the deciding factor. If it is, and traditional aids won’t work, bone conduction might be the solution you’ve been waiting for.
It’s not for everyone. But for the right person - someone who’s tried everything else and still can’t hear clearly - it’s not an alternative. It’s the only real option.
Can bone-conduction hearing aids help with tinnitus?
Bone-conduction devices don’t cure tinnitus, but they can reduce its perception. By delivering external sound directly to the cochlea, they help mask the ringing noise, especially in quiet environments. Many users with single-sided deafness and tinnitus report less annoyance because the brain is no longer focusing on the silence on the deaf side.
Are bone-conduction hearing aids visible?
It depends on the type. Percutaneous systems have a small metal post sticking out of the skin behind the ear - it’s noticeable, especially with short hair. Transcutaneous systems have no external hardware sticking out. The processor clips onto the skin with magnets and can be hidden under hair. Many users choose transcutaneous specifically to avoid drawing attention.
How long do bone-conduction devices last?
The implanted part - the titanium screw or magnet - is designed to last a lifetime. The external sound processor typically lasts 5-7 years, depending on usage and maintenance. Batteries need replacing every few days, and processors can be upgraded without another surgery. Newer models support wireless updates, so you can get new features without buying a whole new device.
Can children use bone-conduction hearing aids?
Yes - and they’re often the best option for kids with congenital ear malformations. Children as young as 5 can get implantable systems. Before that, a softband version holds the processor against the skull with a headband. This allows early sound exposure, critical for speech development. Studies show kids using bone conduction from age 2-4 develop language skills nearly on par with peers with normal hearing.
Do bone-conduction hearing aids work in water?
The external processors are water-resistant but not waterproof. Most can handle sweat and light rain, but swimming or showering requires removal. Some manufacturers offer waterproof covers or accessories for active users. The implanted part is fully sealed and safe underwater - only the external part needs protection.
What if I need an MRI later?
Most modern bone-conduction implants are MRI-safe up to 1.5 Tesla. You’ll need to remove the external processor before the scan. For 3T MRI machines, the internal magnet may need surgical removal - but it can be reinserted afterward. Always inform your radiologist about your implant before scheduling. Some centers have protocols for scanning patients with these devices safely.
Is there a non-surgical option?
Yes. Softband systems hold the sound processor against the skull with a headband. They’re used for infants, young children, or adults who want to try bone conduction before committing to surgery. They’re not as powerful as implanted systems, but they’re a great way to test if the technology works for you. Many clinics offer rental programs so you can wear one for weeks before deciding.







Write a comment
Your email address will be restricted to us