Switching between blood thinners isn’t just a matter of stopping one pill and starting another. Get it wrong, and you could face a stroke, a pulmonary embolism, or dangerous bleeding. This is where bridging therapy comes in - but only for a small group of people. For most, it’s unnecessary, risky, and outdated.
What Is Bridging Therapy, Really?
Bridging therapy means using a fast-acting injectable blood thinner - like low molecular weight heparin (LMWH) or unfractionated heparin - while temporarily stopping a longer-acting one like warfarin. The goal? To keep your blood from clotting during surgery or a procedure when your regular medication is paused. But here’s the catch: you don’t need it unless you’re at very high risk for clots. Most people on blood thinners today - especially those taking DOACs like apixaban or rivaroxaban - don’t need bridging at all. The idea used to be routine. Now, it’s reserved for just a few.Who Actually Needs Bridging?
Not everyone on warfarin needs a bridge. In fact, only about 10-15% of patients do, based on 2021 guidelines. You might need it if you have:- A mechanical heart valve in the mitral position
- A blood clot in your leg or lung within the last 3 months
- A CHA₂DS₂-VASc score of 5 or higher (for atrial fibrillation) AND a history of stroke or TIA
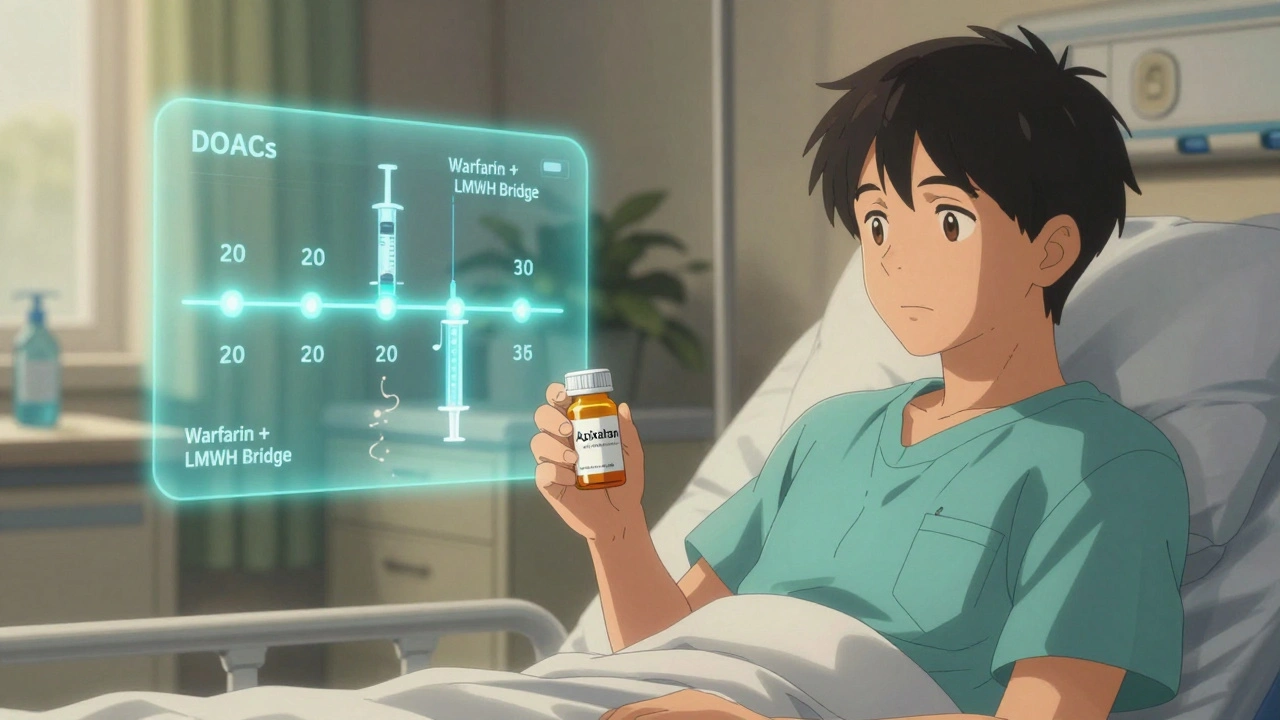
Why DOACs Changed the Game
Direct oral anticoagulants (DOACs) like Eliquis, Xarelto, and Pradaxa are now the go-to for most new patients. Why? They don’t need bridging. Unlike warfarin, which takes days to clear from your body, DOACs leave your system in hours. Apixaban? Half-life is 12 hours. Rivaroxaban? 7-11 hours. Dabigatran? Around 14 hours. That means you can stop them 24-48 hours before surgery, and your blood’s natural clotting ability returns fast enough to make bridging pointless. The 2018 AC Forum guidelines say it clearly: “Bridging is not necessary in DOAC patients due to the rapid onset and offset.” No injections. No daily shots. No extra cost. No increased bleeding risk. In 2023, 75% of new anticoagulant prescriptions were for DOACs. That’s not a trend - it’s the new standard. If you’re still on warfarin, ask why.
How Bridging Works - If You Really Need It
If your doctor says you’re high-risk and need a bridge, here’s what it looks like:- Stop warfarin 5-6 days before your procedure. This lets your INR drop below 2.0.
- Start therapeutic-dose LMWH (like enoxaparin) 3 days before surgery. Usually 1 mg/kg twice daily.
- Stop the LMWH 24 hours before the procedure. For high-bleeding-risk surgeries, sometimes 36-48 hours.
- After surgery, restart LMWH 24-48 hours later - only if there’s no bleeding.
- Restart warfarin the same day you restart LMWH, but at 15-20% higher than your old dose.
- Check your INR in 3-4 days. Adjust as needed.
The Hidden Costs - Beyond Money
Bridging isn’t just risky. It’s expensive and burdensome. A 7-day course of LMWH in the U.S. costs $300-$500. In New Zealand, it’s covered under public health, but you still need to inject yourself twice a day. That’s 14 shots. For many older patients, that’s painful, intimidating, or impossible without help. Studies show 15-20% of patients miss at least one injection. That’s not just non-adherence - it’s a safety gap. One missed dose can mean a clot forms while you’re waiting for the next shot. And then there’s the anxiety. You’re stuck with needles, blood tests, and uncertainty. Meanwhile, DOAC patients just pause their pill, go in for surgery, and restart it the next day.What About Restarting After Surgery?
Restarting your blood thinner after surgery is just as important as stopping it safely. For warfarin: Restart at 15-20% higher than your pre-op dose. Check INR in 3-4 days. Don’t wait until you’re home. Do it while you’re still in the hospital if possible. For LMWH: Restart 24-48 hours after surgery, depending on bleeding risk. Low-risk procedures (like colonoscopy)? 24 hours. High-risk (like brain or spinal surgery)? Wait 48-72 hours. For DOACs: Restart 24 hours after low-bleeding-risk procedures. Wait 48-72 hours after major surgery. Your kidney function matters - if it’s poor, delay longer. Never restart both warfarin and LMWH at the same time without medical supervision. Over-anticoagulation can cause internal bleeding.
Why Doctors Still Overuse Bridging
Despite the evidence, many doctors still bridge too often. Why? Old habits. Fear of lawsuits. Lack of updated training. Some still think, “Better safe than sorry.” But the data says otherwise. The ACC’s “Primum Non Nocere” principle - “first, do no harm” - should guide every decision. Bridging harms more than it helps for most people. A 2020 study found that 60% of patients who got bridged didn’t meet high-risk criteria. That’s overtreating. That’s unnecessary risk. Ask your doctor: “Am I in the 10-15% who need this? Or am I being bridged out of habit?”What You Should Do Right Now
If you’re on a blood thinner and have a procedure coming up:- Know which one you’re on - warfarin or a DOAC?
- Know your CHA₂DS₂-VASc and HAS-BLED scores. Ask your doctor for them.
- Ask: “Do I really need bridging? What’s the evidence for me?”
- If you’re on a DOAC, expect to hear: “No bridge needed.”
- If you’re on warfarin and have no mechanical valve or recent clot, ask why you’re being bridged.
- Make sure your surgeon and pharmacist are on the same page. Write it down. Confirm it.
The Future of Blood Thinners
Bridging therapy is fading. It’s not going away completely - but it’s becoming a relic for a shrinking group. DOACs are cheaper, safer, and easier. Newer anticoagulants are in development with even faster clearance times. In 5 years, bridging may only be mentioned in medical textbooks. For now, the message is clear: If you’re not at very high risk for clots, don’t let anyone talk you into needles, shots, and extra danger. Your body doesn’t need it. The science doesn’t support it. And your safety does.Do I need bridging therapy if I’m on Eliquis or Xarelto?
No. Direct oral anticoagulants (DOACs) like Eliquis and Xarelto leave your system quickly - within hours. You can stop them 24-48 hours before surgery and restart them the same day or next day, depending on bleeding risk. Bridging with injections adds no benefit and increases bleeding risk. This is the standard for 75% of new patients today.
What if I’m on warfarin and need a procedure?
Stop warfarin 5-6 days before surgery. Only start bridging with LMWH if you have a mechanical mitral valve, a clot within the last 3 months, or a CHA₂DS₂-VASc score of 5+ with prior stroke. For most people with atrial fibrillation, bridging isn’t needed. Always check your INR before stopping and after restarting.
Is bridging therapy safe?
It’s not inherently unsafe - but it’s risky for most people. The BRIDGE trial showed a 2.3% major bleeding rate with bridging versus 1.0% without. That’s more than double the risk. For patients not in the highest-risk group, the danger outweighs any benefit. Only use it if your doctor confirms you’re in the 10-15% who truly need it.
How long before surgery should I stop my blood thinner?
For warfarin: stop 5-6 days before. For LMWH: stop 24 hours before. For DOACs like apixaban or rivaroxaban: stop 24-48 hours before. For dabigatran: stop 48 hours before if you have kidney issues. Always confirm timing with your care team - it depends on your procedure and kidney function.
Can I switch from warfarin to a DOAC without bridging?
Yes. When switching from warfarin to a DOAC, stop warfarin and start the DOAC when your INR is below 2.0. No bridging is needed. For the reverse - DOAC to warfarin - start warfarin and a short-acting heparin at the same time, then stop the heparin once the INR is therapeutic. Always do this under medical supervision.



Write a comment
Your email address will be restricted to us