When you’re diagnosed with hormone receptor-positive breast cancer, one of the most important decisions you’ll face is choosing between tamoxifen and aromatase inhibitors. These aren’t just drugs-they’re life-changing treatments that can cut your risk of cancer coming back by a third. But they’re not the same. One works better for younger women. The other is stronger for postmenopausal women. And both come with very different side effects that can change your daily life.
How Hormone Therapy Stops Breast Cancer
Not all breast cancers are the same. About 8 out of 10 are fueled by estrogen. That means the cancer cells have receptors that grab onto estrogen and use it to grow. Hormone therapy blocks that process. It doesn’t kill cancer cells outright-it starves them.
Tamoxifen has been around since the 1970s. It works like a key that fits into estrogen receptors but doesn’t turn them on. Instead, it blocks estrogen from getting in. Aromatase inhibitors (AIs) do something completely different. They shut down the body’s main source of estrogen after menopause. The enzyme aromatase turns male hormones into estrogen. AIs like anastrozole, letrozole, and exemestane stop that conversion, cutting estrogen levels by 95% or more.
This difference matters because your body makes estrogen differently before and after menopause. Before menopause, your ovaries produce most of it. After, fat tissue and other organs take over using aromatase. That’s why tamoxifen is the go-to for premenopausal women, and AIs are the standard for postmenopausal women.
Which One Works Better? The Evidence
Large studies involving tens of thousands of women have answered this question clearly.
For women who’ve gone through menopause, aromatase inhibitors reduce the risk of cancer returning by about 30% more than tamoxifen over five years. In one major study, 12.1% of women on AIs died from breast cancer after 10 years, compared to 14.2% on tamoxifen. That’s not a huge difference in percentage points-but when you’re talking about thousands of women, it means hundreds of lives saved.
For younger women, it’s more complicated. AIs alone don’t work because the ovaries still make estrogen. But if you add ovarian suppression-using drugs like goserelin to temporarily shut down the ovaries-then AIs become more effective than tamoxifen. The TEXT and SOFT trials showed that combining exemestane with ovarian suppression reduced recurrence risk by 21% compared to tamoxifen with ovarian suppression. For every 31 women treated this way, one extra recurrence was prevented.
But here’s the catch: the biggest benefit of AIs happens in the first 4 to 5 years. After that, the gap narrows. That’s why some doctors recommend switching from tamoxifen to an AI after 2 or 3 years-especially if you’re postmenopausal. Real-world data shows this approach gives nearly the same results as starting with an AI right away.
The Side Effects You Can’t Ignore
Both drugs save lives-but they also change your body in ways that can be hard to live with.
Tamoxifen carries a higher risk of blood clots and stroke. It also slightly increases the chance of endometrial cancer-about 1.2% over 10 years, compared to 0.4% with AIs. That’s why women on tamoxifen need regular pelvic exams.
Aromatase inhibitors, on the other hand, are brutal on bones and joints. Because they drop estrogen so low, bone density falls faster. Studies show 6.4% of women on AIs break a bone over 10 years, compared to 5.1% on tamoxifen. Joint pain is even more common-about half of women on AIs report moderate to severe pain in their hands, knees, or back. One in five stops taking the drug because of it.
On the flip side, tamoxifen users often deal with hot flashes, night sweats, and mood swings. In online patient forums, 63% of tamoxifen users say hot flashes are their biggest issue. AI users complain more about brain fog and fatigue. One Reddit thread summed it up: “Tamoxifen made me feel like I was burning up. AIs made me feel like my bones were turning to dust.”
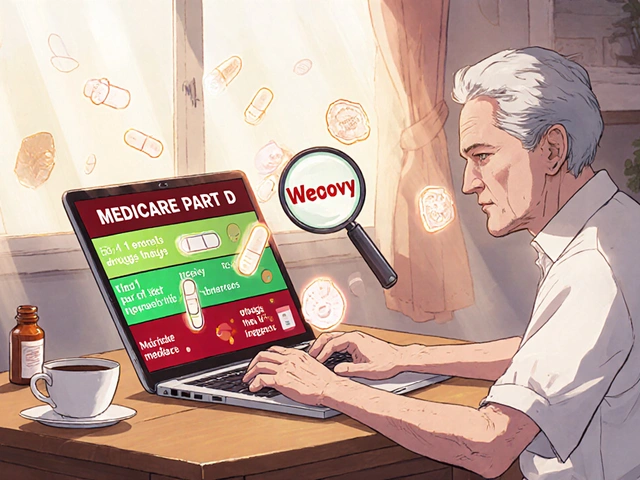
And then there’s the cost. Tamoxifen is a generic pill that costs about $15 a month. Aromatase inhibitors? Even generic versions can run $100 to $150 a month. That’s a huge burden for people without good insurance-and it’s why tamoxifen is still the only option for many women in low-income countries.
Who Gets What? The Rules Doctors Follow
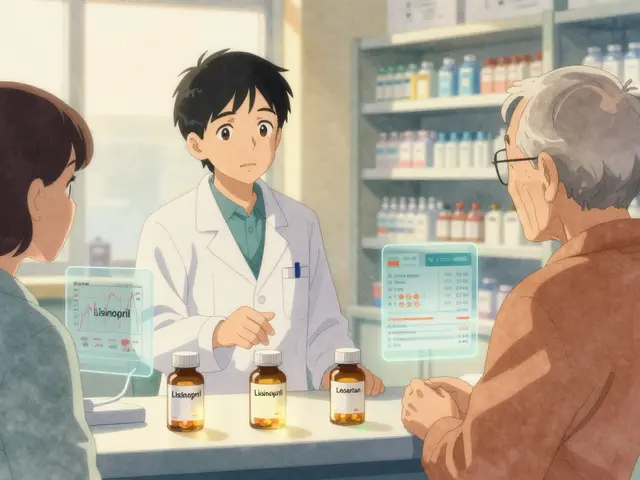
There’s no one-size-fits-all answer. But guidelines from the National Comprehensive Cancer Network (NCCN) and the American Society of Clinical Oncology (ASCO) give clear direction.
For premenopausal women: Tamoxifen is first-line. If you’re high-risk-your tumor is large, high-grade, or spread to lymph nodes-then adding ovarian suppression and switching to an AI is often recommended. The St. Gallen Consensus (2023) says this combo is best for intermediate-to-high risk cases.
For postmenopausal women: Aromatase inhibitors are the standard. You’ll likely take one for 5 to 10 years. Some doctors start with tamoxifen for 2-3 years, then switch to an AI. Others start with the AI right away. The choice often comes down to side effects.
Doctors now use tools like the Oncotype DX test to see how much benefit you’ll get from chemotherapy. If your score is low, you might not need chemo at all-just hormone therapy. That makes choosing between tamoxifen and an AI even more personal.
What About Long-Term Use?
Five years used to be the standard. Now, many women take hormone therapy for 7 to 10 years, especially if their cancer had high-risk features. The MA.17X trial showed that extending AI treatment beyond 5 years cuts recurrence risk even further.
But the longer you take these drugs, the more side effects pile up. That’s why bone health becomes critical. If you’re on an AI, you need a DEXA scan every 1 to 2 years. If your bone density drops too far (T-score below -2.0), your doctor may prescribe zoledronic acid or denosumab to protect your bones.
And here’s something new: in 2023, the FDA approved camizestrant, a new type of hormone drug called a SERD. Early data shows it works better than AIs for tumors with certain mutations. It’s not a first-line option yet-but it’s the first real innovation in this space in over 20 years.

Real People, Real Choices
At the end of the day, this isn’t just about numbers. It’s about your life.
One woman in her early 50s chose an AI because she was terrified of the cancer coming back. She got severe joint pain but stuck with it. “I’d rather hurt than die,” she said.
Another woman, 42 and still having periods, picked tamoxifen because she wanted to keep her bones strong. She knew she’d deal with hot flashes, but she was planning to have kids later. Tamoxifen doesn’t cause infertility like ovarian suppression does.
There’s no right answer. Only the right answer for you. That’s why shared decision-making matters. Your doctor should ask: What are you willing to tolerate? What matters most to you-avoiding recurrence, or avoiding joint pain? What’s your financial situation? Do you have a history of blood clots or osteoporosis?
And if you’re unsure? It’s okay to wait. Some women take tamoxifen for two years, then switch. Others start with an AI and switch if the side effects are too much. The data shows these switches still work.
The Big Picture
Hormone therapy is one of the biggest success stories in cancer care. Since the 1990s, it’s helped cut breast cancer deaths by nearly half in high-income countries. By 2030, it’s expected to prevent 350,000 deaths worldwide each year.
But progress isn’t uniform. In the U.S., 68% of postmenopausal women get AIs. In Japan, tamoxifen is still preferred for women under 70 because of lower fracture rates in Asian populations. In low-income countries, tamoxifen remains the only viable option because of cost.
And research is still moving. The PERSEPHONE trial is testing whether 3 years of tamoxifen works just as well as 5 years for low-risk patients. The CYRILLUS trial is looking at whether testing your genes for CYP2D6 metabolism can help personalize tamoxifen dosing.
For now, the choice between tamoxifen and aromatase inhibitors comes down to your biology, your risk, and your life. Both are powerful. Both have trade-offs. And both have helped millions of women live longer, healthier lives.
Is tamoxifen still used today?
Yes, tamoxifen is still widely used, especially for premenopausal women with hormone receptor-positive breast cancer. It’s also the standard for men with breast cancer and is often chosen when aromatase inhibitors aren’t suitable due to side effects or cost. Generic tamoxifen costs under $20 a month, making it the most accessible option globally.
Can I take aromatase inhibitors if I’m still having periods?
Not on their own. Aromatase inhibitors don’t work if your ovaries are still producing estrogen. But if you combine them with ovarian suppression-using drugs like goserelin to temporarily shut down your ovaries-they become very effective. This combo is now recommended for premenopausal women with higher-risk cancers.
Do aromatase inhibitors cause weight gain?
Weight gain isn’t directly caused by aromatase inhibitors, but many women report it. This is likely due to a combination of factors: lower estrogen levels slowing metabolism, joint pain reducing activity, and aging. Studies show women on AIs gain about 2-4 pounds more over five years than those on tamoxifen. Regular exercise and a balanced diet can help manage this.
How long should I stay on hormone therapy?
Most women take hormone therapy for 5 years. But for those with higher-risk cancer-larger tumors, positive lymph nodes, or high genomic scores-extending treatment to 7-10 years reduces recurrence further. Your doctor will use tools like Oncotype DX and your personal risk factors to decide if longer treatment is right for you.
Can I switch from tamoxifen to an aromatase inhibitor?
Yes, many women do. If you’re postmenopausal and have been on tamoxifen for 2-3 years, switching to an aromatase inhibitor can lower your risk of recurrence even more. Studies show this approach gives results nearly as good as starting with an AI from day one. It’s a common strategy when side effects from tamoxifen become hard to manage.
Are there new alternatives to tamoxifen and aromatase inhibitors?
Yes. In 2023, the FDA approved camizestrant, a new type of hormone drug called a selective estrogen receptor degrader (SERD). It works by breaking down estrogen receptors instead of just blocking them. Early trials show it reduces recurrence by 38% compared to standard therapy in women with ESR1-mutated tumors. It’s not yet a first-line option, but it’s the biggest advancement in this field in over 20 years.




Write a comment
Your email address will be restricted to us