When you’re prescribed a biologic therapy, you’re not just getting a new drug-you’re taking on a new responsibility. These powerful medications, made from living cells, are designed to treat conditions like rheumatoid arthritis, psoriasis, and Crohn’s disease. But unlike pills, they come in pens or syringes you must inject yourself. And if you don’t do it right, you risk more than just a bad day-you risk infection, treatment failure, or even hospitalization.
Why Training Isn’t Just a Formality
Most patients think training means a nurse shows them how to use the pen once, then sends them home. That’s not training. That’s a gamble. A 2022 study found that 91.7% of patients say they received training, but the average session lasted just 30 to 38 minutes. That’s not enough time to learn how to handle a needle, clean your skin properly, or manage anxiety. And worse, one in three patients got no real instruction at all-just a quick verbal rundown. The problem isn’t laziness. It’s system failure. Doctors are overworked. Nurses are stretched thin. Training gets squeezed into the last five minutes of a 20-minute appointment. But here’s the truth: if you don’t know how to inject correctly, your treatment might as well be useless. Studies show that over one-third of patients feel completely unsure about their technique in the first six months. And when you’re unsure, you skip doses. Or you do it wrong. And that’s how treatment stops working-or worse, leads to infection.The Three-Step Training Rule You’re Probably Missing
Effective injection training isn’t about watching. It’s about doing. And it needs three parts: tell, show, and try.- Tell: Someone explains the steps-where to inject, how to hold the pen, what to do if you see blood.
- Show: They demonstrate it on a training device. Not a real needle. Not a placebo. A device that feels exactly like the real one-same weight, same click, same resistance.
- Try: You do it. Right there. In front of them. With their hands ready to guide yours if you panic.
Infection Risk: It’s Not Just About Clean Hands
People think infection means dirty hands. It’s more than that. The CDC says improper injection technique increases infection risk by 37%. Why? Because you’re breaking the skin. Every time. And if you don’t prepare right, bacteria get in. Here’s what actually matters:- Hand hygiene: Wash for 20 seconds with soap. Not 5. Not while you’re distracted. 20 seconds. Sing "Happy Birthday" twice.
- Skin prep: Use an alcohol swab. Let it dry. Don’t blow on it. Don’t wipe it off. Let it air-dry. If you wipe it, you drag bacteria back onto the spot.
- Site rotation: Never inject in the same spot twice. Use your thigh, abdomen, or upper arm. Keep injections at least one inch apart. Reusing the same spot causes tissue damage and increases infection risk.
- Needle safety: Never reuse needles. Even if it looks clean. Biologics are expensive. But your health is priceless.

The Hidden Problem: Anxiety Is Killing Your Treatment
You can do everything right mechanically-and still fail. Why? Because fear messes with your hands. Your heart races. You shake. You rush. You pull the pen away too soon. You forget to press the button. You inject into your clothes. Studies show emotional stress causes 57% of early treatment dropouts-even when patients know the steps. That’s not just psychological. It’s physiological. Your body reacts. And your technique breaks down. The fix? Rituals. Not magic. Not superstition. Routine. A set of small, calming actions that tell your brain: "It’s safe. You’ve done this before. You’re in control."- Always inject at the same time of day.
- Play the same song while you prepare.
- Keep your supplies in the same spot.
- Take three deep breaths before you press the button.
What No One Tells You About Follow-Up
You don’t get one training session. You need three. The first is in the clinic. The second should be a week later. The third, a month after that. Each time, you demonstrate the whole process. The provider watches. They correct. They reassure. And you get better. Patients who had three or more supervised practices retained proper technique at 94% after six months. Those with only one session? Only 52%. That’s almost double the failure rate. And don’t wait for your next appointment. If you’re nervous, call your pharmacist. Many now offer free virtual coaching. Some even send video tutorials with real-time feedback. Use them. Ask for them. Demand them.What’s Changing-And What You Should Expect
The FDA just updated its guidance in early 2023. They’re now pushing manufacturers to provide structured, consistent training tools. Companies like Adbry are already rolling out digital platforms with video demos, virtual coaching, and injection trackers. These aren’t gimmicks. They’re lifelines. But here’s the catch: you have to use them. Don’t just download the app. Open it. Watch the video. Practice with the virtual trainer. Log each injection. The more you engage, the safer you become. Also, ask your provider: "Do you have a standardized training protocol?" If they say no, that’s a red flag. You deserve better. And you’re not asking for too much-you’re asking for what every patient should get.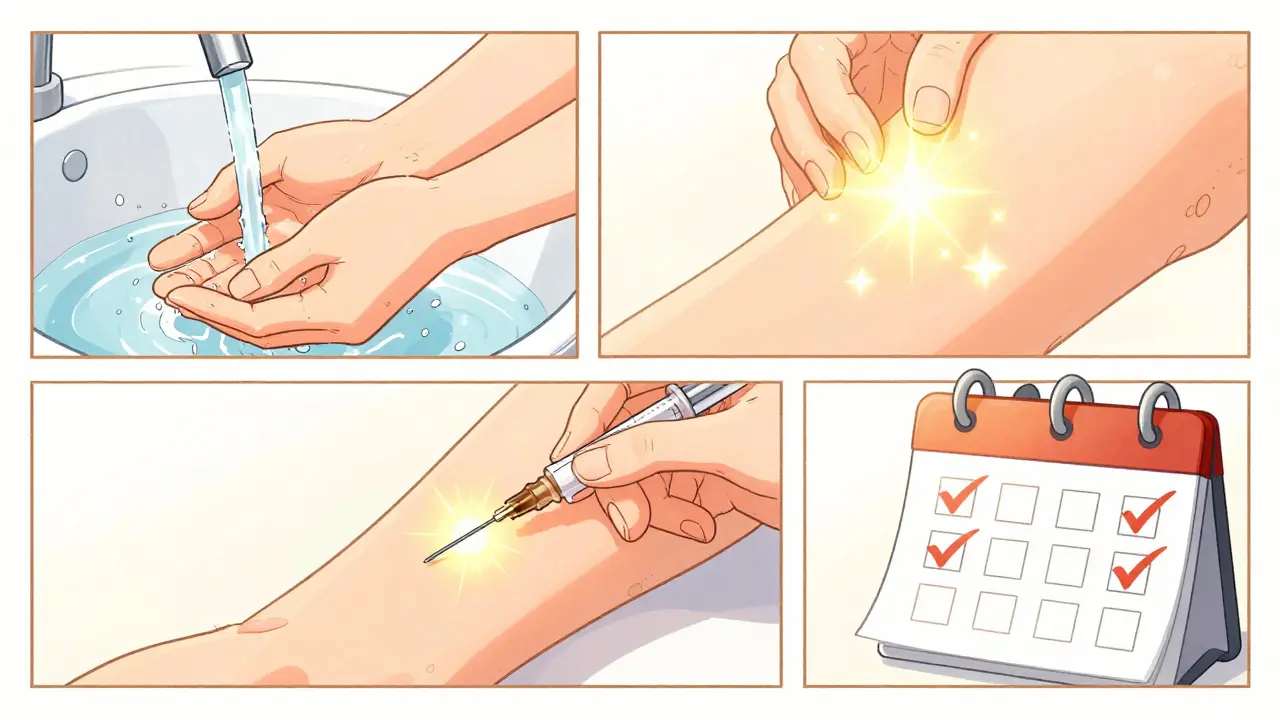
Real Talk: What Patients Are Saying
One Reddit user wrote: "They showed me once. Had me do it once. Sent me home with six months of medication. No follow-up. I cried the first time I tried alone. I was terrified I’d mess up and get sick." That’s not rare. That’s normal. And it’s avoidable. Another patient said: "I started doing the same thing every time-play my favorite song, wipe the spot, breathe, inject. Now I don’t even think about it. It’s just part of my day." That’s the goal. Not perfection. Not fearlessness. Just routine. Consistency. Confidence.Your Action Plan: 5 Steps to Inject Safely
1. Ask for full training before you leave the clinic. Demand the "tell, show, try" method. If they say no, ask for a referral to a pharmacist or nurse educator. 2. Practice daily for a week with a training device. Use a mirror. Record yourself. Watch for shaky hands or rushed movements. 3. Build your ritual. Pick a time, a place, a sound, a breath. Make it yours. 4. Schedule follow-ups. Ask for check-ins at one week, one month, and three months. Don’t wait for them to call you. 5. Know your infection signs. Redness >2cm? Fever? Swelling? Call your doctor immediately. Don’t wait.Final Thought: You’re Not Just Taking Medicine. You’re Managing Your Health.
Biologic therapies are life-changing. But they’re not magic. They only work if you use them right. And using them right isn’t just about the needle. It’s about preparation. Routine. Awareness. And asking for help when you need it. You’ve already taken the hardest step-you said yes to treatment. Now make sure the rest of the journey doesn’t become a risk you didn’t have to take.What happens if I inject into a bruise or scar?
Never inject into a bruise, scar, or inflamed skin. These areas have poor blood flow and damaged tissue, which can delay medication absorption and increase infection risk. Always choose clean, healthy skin at least one inch away from any previous injection site.
Can I reuse my training device?
Yes. Training devices are designed for repeated use and contain no medication. They’re meant to help you practice technique, not deliver treatment. Clean them with mild soap and water after each use, and store them in a dry place.
Is it safe to inject in public places like airplanes or restrooms?
It’s possible, but not ideal. Public restrooms are high-risk environments for contamination. If you must inject on the go, carry a clean alcohol wipe and a small disposable surface (like a paper towel or tissue) to place your supplies on. Always wash your hands first, and avoid touching surfaces before handling the device.
Why do some biologics come in pens and others in syringes?
Pens are designed for ease and safety-they conceal the needle and often have auto-injection features. Syringes require more manual control and are typically used for higher doses or less common formulations. The choice depends on the drug’s properties and manufacturer design. Your provider will match the delivery method to your needs.
What should I do if I drop my biologic pen or syringe?
If the device hits the floor or any unclean surface, do not use it. Even if the needle looks clean, it may have picked up bacteria. Contact your pharmacy or provider for a replacement. Never risk an infection by using a contaminated device.
Can I get an infection even if I follow all the rules?
Yes. No method is 100% foolproof. But following proper technique reduces your risk by more than 60%. Infections are rare when you wash your hands, prep your skin, rotate sites, and avoid contamination. If you’re still concerned, talk to your doctor about your personal risk factors-like diabetes or a weakened immune system.







Write a comment
Your email address will be restricted to us