When a drug recall happens, time isn’t just money-it’s lives. A single misplaced pill with the wrong lot number can lead to serious harm, or worse. In 2022, over 7,100 drug recalls were issued in the U.S. alone, mostly because of manufacturing defects like contamination, incorrect dosing, or faulty packaging. If you’re a pharmacist, nurse, or hospital staff member, you can’t afford to wait for a memo or hope someone else handled it. You need a clear, reliable system to verify recall notices and confirm which medication lots are affected-and act fast.
Don’t Trust Just One Source
Relying on a single channel to get recall notices is a dangerous habit. The FDA doesn’t send out one official email or letter. You’ll get alerts through multiple channels: FDA’s MedWatch portal, manufacturer notifications, pharmacy distributor alerts, state health department bulletins, and even industry services like First Databank or Grayson’s RecallTrac. A 2022 survey of hospital pharmacists found that 78% received conflicting lot numbers across these sources. One email says Lot A123 is affected. A fax says A124. A text alert says A123 and A125. That’s not confusion-it’s a risk.Best practice? Set up a system where you receive every notice. Subscribe to FDA’s MedWatch alerts, sign up for distributor recall feeds, and ensure your pharmacy management system pulls in real-time updates from trusted third-party sources. Never wait for the mail. In 2023, the FDA found that 41% of verification failures came from unopened emergency kits that were never checked because no one thought to look there.
Know the Three Classes of Recalls
Not all recalls are the same. The FDA classifies them based on risk:- Class I: Highest risk. Use of the product could cause serious injury or death. Think contaminated injectables or pills with 10x the intended dose.
- Class II: May cause temporary or medically reversible health problems. Could include mislabeled pills or packaging with expired dates.
- Class III: Unlikely to cause harm but violates FDA labeling or manufacturing rules. Think incorrect font size on a label.
Your response time changes with the class. For Class I recalls, you have 48 hours to verify and remove all affected lots-no exceptions. The FDA’s 2023 update to 21 CFR 7.50 made this official. For Class II, you have up to 72 hours. Class III still needs action, but the urgency is lower. Knowing the class tells you how hard and fast to move.
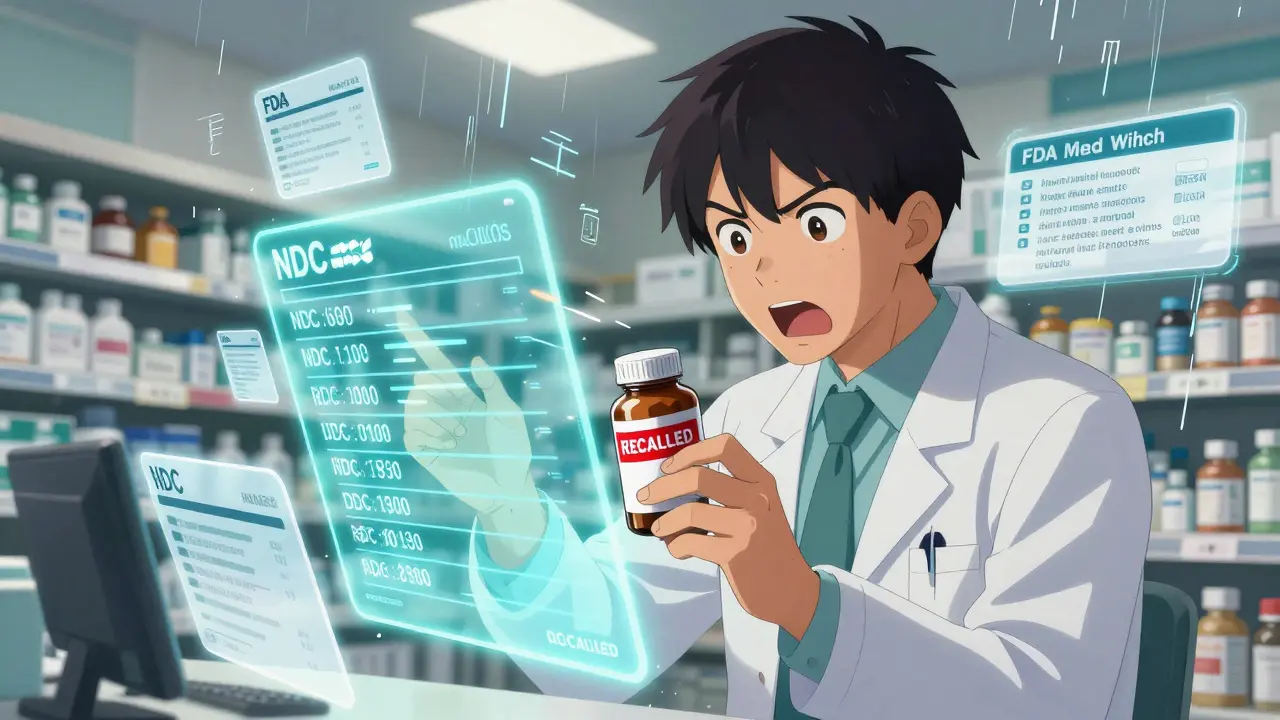
Verify Using the Exact Product Identifiers
You can’t just look at the drug name. You need four exact matches:- National Drug Code (NDC): The 10- or 11-digit number on the package. It’s unique to the manufacturer, strength, and package size.
- Lot number: Usually printed near the expiration date. It’s a batch identifier. Even if two bottles have the same NDC, different lot numbers mean different production runs.
- Expiration date: Some recalls only affect batches expiring in a certain window.
- Package size: A 30-count bottle might be recalled, but the 100-count version isn’t.
One hospital in California missed a Class I recall because their staff checked only the NDC and assumed all lots were affected. They didn’t cross-check the lot numbers-and kept 147 bottles of the safe version on the shelf. That’s not an error. That’s negligence.
Use your pharmacy software to search by NDC and lot number together. If your system doesn’t allow that, print out the recall notice and manually compare every bottle in stock. Don’t skip the back shelves, the storage room, or the crash cart. The FDA’s audit found that 68% of hospitals failed to check emergency supplies.

Remove and Quarantine Immediately
Once you confirm a lot is affected, take it out of circulation-right away. Move it to a secure, labeled quarantine area. Don’t just put it in a drawer. Don’t wait until the end of your shift. For Class I recalls, removal must happen within 24 hours. That’s a Joint Commission requirement, not a suggestion.Tag every recalled item with a red sticker that says “RECALLED-DO NOT DISPENSE.” Log the exact quantity removed by lot number. If you have 12 bottles of Lot B456, write it down. If you’re unsure, count again. Documentation isn’t paperwork-it’s legal protection. The FDA fined one clinic $84,350 in 2022 because they couldn’t prove they removed all affected lots.
Find Alternatives and Notify Patients
You can’t just take the drug off the shelf and leave patients without treatment. Immediately identify safe alternatives. Check your inventory for the same drug from a different manufacturer or lot. If you don’t have it, contact your wholesaler or another facility. Many hospitals now have reciprocal agreements to share stock during recalls.If the drug was given to patients-especially inpatient or long-term care-you must notify them. For Class I recalls, you’re required to contact 100% of direct patients who received the affected product. That means calling, mailing, or texting them. Don’t rely on your EHR to do it automatically. A 2023 study showed that 37% of recalls were missed because facilities assumed their electronic records had the right patient data. They didn’t. Always verify patient contact info manually.
Automated Systems Save Time-and Lives
Manual verification is slow and error-prone. A 2022 ASHP study found that pharmacists spent an average of 4.7 hours per recall using paper lists and spreadsheets. The error rate? 18.3%. That means nearly 1 in 5 recalls had mistakes.Automated systems like TruMed’s AccuSite or Navitus’ Recall Management Platform cut that time to under 1.2 hours and reduce errors to 2.1%. These tools integrate with your pharmacy software and flag recalled items the moment someone tries to dispense them. They auto-match NDCs and lot numbers against real-time recall databases. One hospital in Minnesota reduced their recall response time from 4.5 hours to 22 minutes after switching to an automated system.
But automation isn’t for everyone. If you’re a small rural pharmacy with outdated systems, these tools might be too expensive or too complex. Grayson’s RecallTrac requires at least 50 users to be cost-effective. First Databank costs $4,800 a year. For smaller clinics, a well-organized checklist and a dedicated person responsible for recalls can still work-if they’re followed strictly.
Document Everything
You must keep records of every step. The Joint Commission requires proof of:- Date and time you received the recall notice
- Lot numbers verified and removed
- Quantities quarantined and returned
- Staff who were notified
- Patients contacted and how
- Alternative medications provided
- Proof of effectiveness checks (for Class I recalls)
Don’t use sticky notes. Use a digital log or a printed recall verification form. Store it for at least five years. If the FDA audits your facility, they’ll ask for this. If a patient is harmed and you can’t prove you acted, you’re liable.
Train Your Team and Build a Playbook
Recall verification isn’t a one-person job. You need a team. The ASHP recommends forming a dedicated Recall Team with clear roles: who gets the alerts, who checks inventory, who contacts patients, who documents everything. Facilities with formal teams completed verification 3.2 times faster than those without.Create a “recall playbook.” It’s a simple one-page document that answers:
- Who to call first when a recall comes in?
- Where are the quarantine bins?
- Which software do we use to check lots?
- What’s the phone list for patient notifications?
- How do we log actions?
86% of top-performing pharmacies use one. The best ones are posted on the wall near the pharmacy counter. They’re updated every quarter. New staff get trained on them during orientation.
What’s Changing in 2026?
The rules are getting stricter. By 2027, the Drug Supply Chain Security Act will require all prescription drugs to have electronic verification at every step. The FDA is already testing AI-powered lot-matching tools in 12 academic hospitals. These systems can scan a bottle’s barcode, compare it to a live recall database, and flag mismatches before the pill even leaves the shelf.Pfizer and Walgreens are testing blockchain systems that track every batch from factory to pharmacy. In their 2023 trial, verification time dropped to 17 minutes. That’s the future.
Right now, your job is to make sure you’re not left behind. Whether you use software or paper, the steps are the same: get the notice, check the NDC and lot, remove it, notify patients, document it. Skip one step, and you risk more than a fine. You risk someone’s life.




Write a comment
Your email address will be restricted to us