When your hands feel clumsy, your balance goes off, or you start tripping over nothing, it’s easy to blame aging. But if these symptoms are getting worse-especially if you’re over 55-it could be something more serious: cervical myelopathy. This isn’t just a stiff neck or occasional numbness. It’s the spinal cord in your neck being squeezed, and left untreated, it can lead to permanent weakness, loss of coordination, or even paralysis.
What Exactly Is Cervical Myelopathy?
Cervical myelopathy happens when the spinal cord in your neck gets compressed. The most common cause? Cervical spinal stenosis-the narrowing of the bony canal that protects your spinal cord. Think of it like a tunnel that’s slowly shrinking. Over time, bone spurs grow, discs flatten, ligaments thicken, and the space for your spinal cord gets tighter. When the canal drops below 13mm in width (normal is 17-18mm), it starts pressing on the cord. That’s when symptoms appear.This isn’t just about pain. It’s about function. The spinal cord carries signals from your brain to your arms, legs, and organs. When it’s compressed, those signals get scrambled. That’s why people with cervical myelopathy don’t just feel pain-they lose control. They drop things. They stumble. They can’t button shirts. They might suddenly need to urinate more often. These aren’t random quirks. They’re red flags.
Early Warning Signs You Can’t Ignore
The symptoms of cervical myelopathy don’t show up all at once. They creep in. Many people dismiss them as "getting older." But here’s what to watch for:- Hand clumsiness: You drop keys, fumble with zippers, or struggle to turn doorknobs. This happens because the nerves controlling fine motor skills in your hands are being compressed.
- Gait instability: Walking feels off. You feel unsteady, like you’re walking on a boat. You might drag your feet or catch your toes on the floor.
- Increased reflexes: Your doctor might notice your knee or ankle reflexes are overly active during a checkup. This is one of the earliest clinical signs.
- Numbness or tingling: Not just in your fingers, but often radiating down your arms or into your legs.
- Bladder changes: Urgency or difficulty emptying your bladder. This is a late sign-but when it shows up, it means the damage is significant.
Studies show that 72% of patients report hand clumsiness first. By the time gait problems appear, the condition has often been progressing for months-even years. And here’s the hard truth: 63% of people with untreated cervical myelopathy get worse over two years. Only 28% improve on their own.
How Is It Diagnosed?
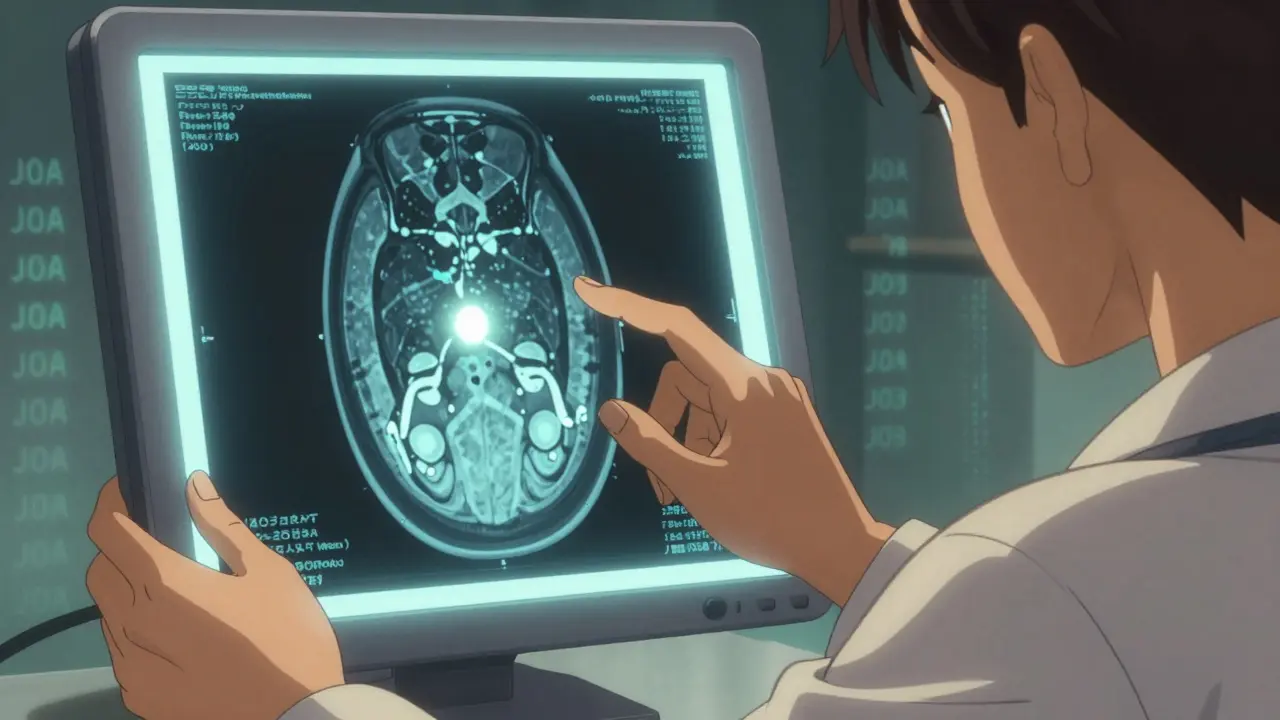
A simple X-ray won’t cut it. You need an MRI. That’s the gold standard. It shows not just the narrowing of the canal, but also whether the spinal cord itself is damaged. Look for T2-weighted hyperintensity-a bright spot on the MRI that signals cord injury. Without that, you might just have stenosis. With it? You have myelopathy.Doctors also use the Japanese Orthopaedic Association (JOA) score. It’s a simple 17-point test that checks your arm and leg movement, sensation, and bladder control. A score below 14 means myelopathy is present. It’s not perfect, but it’s reliable. And it helps track progress-if you’re getting worse, it shows up here.
CT myelography and nerve tests like EMG or SSEPs can help too, especially if an MRI isn’t possible. But in most cases, the MRI is enough. The problem? Many patients wait too long. On average, it takes 14.3 months to get the right diagnosis. By then, the spinal cord may already be permanently damaged.
When Is Surgery the Only Real Option?
Conservative treatment-physical therapy, NSAIDs, activity changes-might help a little. But for moderate to severe myelopathy (JOA score below 12), surgery is the only thing that reliably stops progression and restores function.Here’s what the data says: 70-85% of patients who have surgery see meaningful neurological improvement. Compare that to just 29% of people who avoid surgery and still manage to improve after two years. The difference isn’t close.
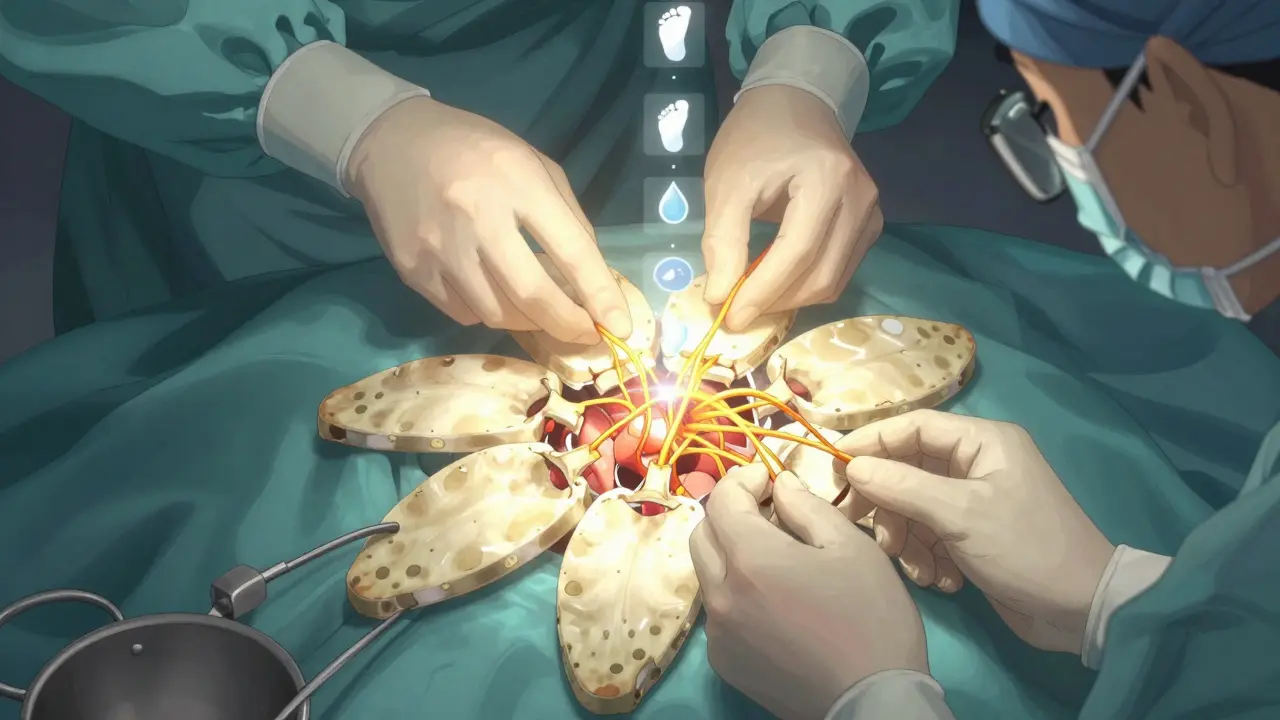
There are three main surgical approaches:
- Anterior Cervical Discectomy and Fusion (ACDF): The surgeon goes in from the front, removes the damaged disc and bone spurs, then fuses the vertebrae. Best for single-level disease. Success rate? Around 90% patient satisfaction. But 5-7% of people develop problems in nearby discs within 10 years.
- Laminectomy with Fusion: The back of the spine is opened to relieve pressure. Then the vertebrae are fused. This is used for multi-level disease or when the spine is unstable. Neurological recovery is strong-up to 85%.
- Laminoplasty: Instead of removing bone, the surgeon opens the back of the spinal canal like a door. Preserves motion. Less postoperative neck pain. Recovery is slightly slower than fusion, but great for patients with 3 or more affected levels.
There’s also cervical disc replacement-a newer option. The FDA approved the M6-C disc for two- to three-level use in 2023. Early results show 81% of patients kept spinal motion at two years, compared to 63% with fusion. It’s promising, but not for everyone.
Timing Matters More Than You Think
This is critical: delaying surgery hurts outcomes.Studies show that patients who have surgery within six months of symptom onset recover 37% better than those who wait over a year. For every month you wait, your chance of full recovery drops by about 3%. Why? Because the spinal cord doesn’t regenerate well. Once nerve fibers are crushed or scarred, they don’t bounce back.
One patient survey found that people treated early were 2.7 times more likely to report "excellent" outcomes on the JOA scale. That’s not a small difference. That’s life-changing.
But surgery isn’t risk-free. About 4-6% of people face major complications: swallowing trouble (dysphagia), nerve damage (C5 palsy), or even worsening symptoms. About 22% of ACDF patients have trouble swallowing for the first few months. Around 35% still have neck pain six months later. And 18% of those who have posterior surgery develop chronic axial neck pain-sometimes called post-laminectomy syndrome.
That’s why choosing the right surgeon matters. Surgeons who do more than 50 cervical procedures a year have 32% fewer complications. Experience counts.
What Happens After Surgery?
Recovery isn’t quick. You’re not back to normal in a week. Most people stay in the hospital 1-3 days, depending on the approach. Then comes rehab.Eighty-five percent of patients need formal physical therapy for 8-12 weeks. Therapy focuses on gait training, balance, and strengthening the neck and core. Without it, you’re more likely to fall or lose progress.
Pre-op prep matters too. If you smoke, quit. Smoking cuts fusion success rates by half. If you’re diabetic, get your HbA1c under 7.0. That drops infection risk from 8.5% to 3.2%. These aren’t small tweaks-they’re game-changers.
What’s Next for Treatment?
The field is moving fast. Minimally invasive laminoplasty, developed in 2021, cuts blood loss by 65% and shortens hospital stays by nearly two days. Robotic-assisted surgery is on the horizon-expected to become standard for complex cases by 2030, reducing revision rates from over 10% to under 7%.Researchers are even testing drugs like riluzole, used in ALS, to protect nerves during surgery. Early trials show a 12% boost in recovery speed when combined with surgery.
But there’s a warning. Surgeon Zorica Buser points out that cervical spine surgeries have jumped 33% since 2010, without better selection criteria. About 15-20% of these procedures might be unnecessary. That’s why diagnosis needs to be tight: symptoms must match imaging. No guesswork.
What Should You Do If You Suspect Cervical Myelopathy?
If you’re over 55 and noticing hand clumsiness, unexplained balance issues, or worsening numbness in your arms or legs, don’t wait. See a spine specialist. Get an MRI within two to four weeks of noticing symptoms. Don’t let a delay cost you your mobility.Surgery isn’t a last resort-it’s a timely intervention. The goal isn’t just to stop the decline. It’s to regain what you’ve lost. And the sooner you act, the better your odds.




Write a comment
Your email address will be restricted to us