When you're in your late 40s or early 50s and suddenly can't sleep because of night sweats, or you're walking into a meeting drenched in sweat at 9 a.m., you start wondering: is this just aging, or is there something you can actually do about it? For millions of women, Hormone Replacement Therapy (HRT) is the answer-but it’s not simple. It’s not a one-size-fits-all pill. It’s a medical decision that needs to be made with clear eyes, updated information, and a plan for ongoing care.
What HRT Actually Does
HRT replaces hormones your body stops making after menopause-mainly estrogen, and sometimes progesterone. Estrogen drops sharply when your ovaries slow down, and that’s what triggers hot flashes, vaginal dryness, sleep problems, and even mood swings. For some women, these symptoms are mild. For others, they’re debilitating. The goal of HRT isn’t to reverse aging. It’s to relieve symptoms so you can live normally again. Studies show it reduces hot flashes and night sweats by 80-90%, far more effectively than antidepressants like SSRIs, which typically cut them by only 50-60%. It also helps protect your bones. Women on HRT have a 34% lower risk of fractures compared to those who don’t take it. That’s not small. Osteoporosis isn’t just about being frail-it’s about breaking a hip at 65 and never walking the same way again.The Big Shift: Why HRT Got a Bad Reputation
In 2002, the Women’s Health Initiative (WHI) study shook the medical world. It found that women taking a combination of estrogen and progestin had a slightly higher risk of breast cancer, heart attacks, strokes, and blood clots. Overnight, prescriptions dropped by more than half. Many women stopped HRT out of fear. Doctors stopped offering it. But here’s what got lost in the noise: the women in that study were mostly over 60, and many had been through menopause for over 10 years. They weren’t the people HRT was meant for. The real benefit-risk balance flips completely when you start HRT before 60, or within 10 years of your last period. That’s called the “timing hypothesis.” New data from the North American Menopause Society (NAMS) and the FDA (updated in 2022) now clearly say: for women under 60 with moderate to severe symptoms, the benefits outweigh the risks. Heart disease risk drops by 32% when HRT starts early. Stroke and clot risks? They’re still there-but they’re much lower with certain forms of HRT.Types of HRT: Oral, Patch, Gel, Vaginal
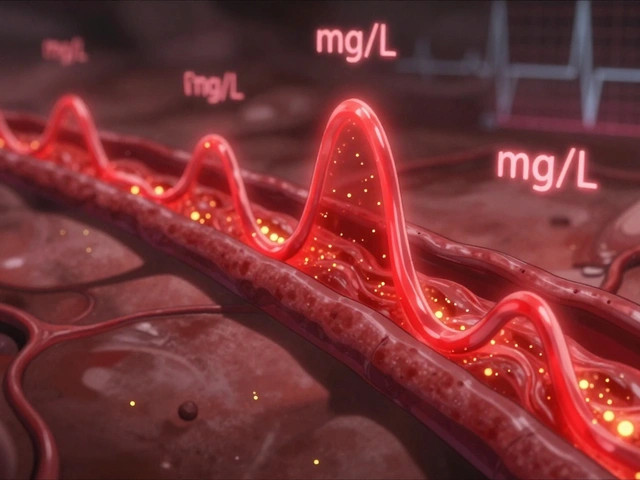
Not all HRT is the same. How you take it changes everything. Oral pills (like Premarin or estradiol tablets) are the most common-but they’re also the riskiest. When swallowed, hormones go straight to the liver, which can increase clotting factors. The risk of deep vein thrombosis (DVT) is about 3.7 per 1,000 women per year with oral estrogen. Transdermal options (patches, gels) bypass the liver. They deliver estrogen through the skin. That cuts DVT risk nearly in half-down to 1.3 per 1,000 women per year. Many women report fewer side effects too: less nausea, less bloating. A 2020 study found 68% of transdermal users were still on HRT after a year, compared to just 52% of pill users. Vaginal estrogen (rings, tablets, creams) is for women whose main issue is dryness, pain during sex, or frequent UTIs. It’s local, low-dose, and doesn’t affect the rest of your body. No increased cancer or clot risk. You can use it for years without worry. If you still have a uterus, you must take progesterone (or a progestin) along with estrogen. Otherwise, you risk endometrial cancer. Micronized progesterone (like Prometrium) is preferred over synthetic progestins-it’s closer to your body’s natural hormone and carries a lower breast cancer risk.The Breast Cancer Question
This is the biggest fear. And it’s real-but not as scary as people think. The WHI study found a 26% increased risk of invasive breast cancer with estrogen-plus-progestin after 5.6 years. That sounds alarming. But let’s put it in perspective: the absolute increase was about 8 extra cases per 10,000 women per year. That’s less than 1%. And here’s the twist: estrogen-only therapy (for women without a uterus) shows no increased breast cancer risk-even after 10 years of use. The risk comes mostly from the progestin part. Also, newer data from 2024 suggests that bioidentical hormones (molecularly identical to human hormones) may carry lower risks than older synthetic versions. But beware: compounded “bioidentical” creams from specialty pharmacies aren’t FDA-approved. They’re not tested for consistency or safety. Stick to regulated products: FDA-approved estradiol patches, micronized progesterone pills, or gels.
Who Should NOT Take HRT
HRT isn’t for everyone. You should avoid it if you have:- A history of breast cancer
- Active blood clots or a history of deep vein thrombosis or pulmonary embolism
- Unexplained vaginal bleeding
- History of stroke or heart attack
- Severe liver disease
Monitoring: What You Need to Do Regularly
Starting HRT isn’t a one-time prescription. It’s an ongoing partnership with your doctor. Before you start:- Baseline mammogram
- Breast exam
- Pelvic exam
- Blood pressure check
- BMI measurement
- Breast exam
- Blood pressure check
- Weight and symptom review
- Discuss whether you still need HRT
What If You Want to Stop?
Many women stop HRT because they’re scared. Others stop because their symptoms fade. That’s okay. But don’t just quit cold turkey. If you’ve been on HRT for more than a year, taper slowly over 2-3 months. Stopping abruptly can bring back hot flashes with a vengeance-and sometimes worse than before. And here’s something no one tells you: if you stop HRT, your bone loss speeds up again. That’s why some women stay on low-dose estrogen for years, especially if they have osteoporosis. It’s not forever-it’s as long as you need it.
Alternatives to HRT
Not everyone wants hormones. That’s fine. For hot flashes, low-dose SSRIs like paroxetine (Brisdelle) can help-but they’re about half as effective as HRT. Gabapentin and clonidine are other options, but they come with drowsiness or dry mouth. For bone health, weight-bearing exercise, vitamin D, calcium, and bisphosphonates (like alendronate) are good. But they don’t touch hot flashes or vaginal dryness. For vaginal symptoms, non-hormonal lubricants and moisturizers help-but they don’t rebuild tissue the way low-dose estrogen does. HRT still wins for comprehensive symptom relief.The Future of HRT
Science is moving fast. In 2023, researchers found that your genes can predict how well you metabolize estrogen. A variant in the CYP1B1 gene means you might need a lower or higher dose. Personalized dosing is coming. New drugs like Duavee (conjugated estrogens + bazedoxifene) offer estrogen benefits without stimulating the uterus-no progestin needed. Clinical trials show a 76% drop in endometrial thickening compared to estrogen alone. Transdermal progesterone is in development. Right now, oral progesterone causes drowsiness and mood swings in some women. A patch or gel version could change that. And yes, the market is growing. After years of decline, HRT prescriptions in the U.S. rose from 9.4 million in 2003 to 15.7 million in 2022. More women are asking for it. More doctors are prescribing it correctly.Final Thoughts: Is HRT Right for You?
Ask yourself:- Are my symptoms disrupting my life-sleep, work, relationships?
- Am I under 60, or within 10 years of menopause?
- Do I have any major health conditions that make HRT unsafe?
- Am I willing to get regular checkups and stay in touch with my doctor?
Start low. Go slow. Monitor. Reassess every year. And don’t let old fears stop you from living well today.
Is hormone replacement therapy safe for women over 60?
For women over 60 who haven’t started HRT, it’s generally not recommended unless they have severe, persistent symptoms and no other options. The risks of stroke, blood clots, and breast cancer increase with age, and the heart-protective benefits no longer apply if HRT is started more than 10 years after menopause. If you’re over 60 and already on HRT, your doctor may recommend tapering off unless you have osteoporosis or severe vaginal atrophy that hasn’t responded to local treatments.
Does HRT cause weight gain?
HRT itself doesn’t cause weight gain. Weight gain during menopause is mostly due to aging, reduced muscle mass, and slower metabolism. Some women report bloating or water retention when starting HRT, especially with oral pills, but this usually fades. Transdermal forms are less likely to cause this. Maintaining a healthy diet and regular exercise is still the best way to manage weight during and after menopause.
How long should I stay on HRT?
There’s no fixed time limit. Most women take HRT for 2-5 years to manage symptoms. But if you have severe osteoporosis, persistent hot flashes, or early menopause (before 45), you may benefit from staying on it longer-sometimes into your 60s or 70s. The key is annual reviews with your doctor to weigh ongoing benefits against risks. Never stop abruptly; taper slowly to avoid rebound symptoms.
Are bioidentical hormones safer than synthetic ones?
FDA-approved bioidentical hormones-like estradiol patches or micronized progesterone-are identical to what your body makes and are considered safe when used as directed. But compounded bioidentical hormones, made in specialty pharmacies, are not FDA-regulated. They vary in strength, purity, and absorption. There’s no strong evidence they’re safer or more effective than standard HRT. Stick to FDA-approved products for consistency and safety.
Can I use HRT if I’ve had breast cancer?
Generally, no. Estrogen can fuel certain types of breast cancer. Most oncologists advise against HRT for women with a history of estrogen-receptor-positive breast cancer. However, for women with severe vaginal symptoms who can’t use non-hormonal options, low-dose vaginal estrogen may be considered under strict supervision. Always consult your oncologist before considering any hormone therapy after breast cancer.
What’s the best way to start HRT?
Start with the lowest effective dose of transdermal estradiol (patch or gel) if you have a uterus, and add micronized progesterone if needed. For example, a 0.025mg estradiol patch or 0.5mg daily gel, plus 100-200mg micronized progesterone nightly for 12-14 days each month. Avoid starting with oral pills unless you have a specific reason. Give it 3 months to settle, then reassess with your doctor. Don’t rush into higher doses.
Does HRT improve mood or depression?
HRT can improve mood in women whose depression or irritability is directly tied to menopause symptoms like sleep disruption and hot flashes. It’s not an antidepressant, but for some, stabilizing hormone levels lifts brain fog and emotional swings. If you have clinical depression, you’ll still need therapy or medication-HRT alone won’t fix it.
Will HRT make me look younger?
HRT doesn’t reverse aging or erase wrinkles. But it can help maintain skin thickness, elasticity, and moisture by supporting collagen production. Many women report their skin feels less dry and more resilient on HRT. This is a side benefit-not the main goal. Don’t start HRT just to look younger; it’s not worth the risk.
Next Steps: What to Do Now
If you’re considering HRT:- Track your symptoms for a month-note frequency and severity of hot flashes, sleep issues, mood changes.
- Get your blood pressure checked and ask for a mammogram if it’s been over a year.
- Find a provider experienced in menopause care-not every GP is up to date on current guidelines.
- Ask about transdermal options first. Ask about micronized progesterone, not synthetic progestins.
- Set a 3-month follow-up. Don’t wait until you’re having side effects to speak up.




Write a comment
Your email address will be restricted to us