Antibiotic Eye Drop Decision Tool
Step 1: Infection Severity
Step 2: Suspected Bacteria
Step 3: Patient Factors
Step 4: Local Resistance Patterns
Step 5: Cost Considerations
Quick Takeaways
- Ciloxan delivers 0.3% ciprofloxacin, a broad‑spectrum fluoroquinolone ideal for bacterial conjunctivitis and corneal ulcers.
- Alternatives such as moxifloxacin, ofloxacin, and tobramycin differ in spectrum, dosing frequency, and resistance profiles.
- For mild infections, azithromycin eye drops offer once‑daily dosing and good tolerability.
- When resistance to fluoroquinolones is suspected, aminoglycosides (e.g., gentamicin) become a useful backup.
- Choosing the right drop depends on infection severity, local resistance patterns, patient adherence, and cost.
Eye infections are common, but the right antibiotic can make the difference between a quick recovery and a lingering problem. Ciloxan Ophthalmic Solution is a 0.3% ciprofloxacin hydrochloride eye drop marketed for bacterial conjunctivitis, keratitis, and corneal ulcers. It belongs to the fluoroquinolone class, which penetrates ocular tissues well and works against a wide range of Gram‑negative and Gram‑positive bacteria.
But Ciloxan isn’t the only option on the shelf. In many clinics you’ll also see moxifloxacin (Vigamox), ofloxacin (Ocuflox), tobramycin (Tobrex), and even azithromycin (Azyter). Each has its own set of strengths, dosing schedules, and resistance concerns. This guide walks you through the most relevant alternatives, compares key attributes, and helps you decide when to stick with Ciloxan and when another drop might be a better fit.
How Ciprofloxacin Works in the Eye
When you administer Ciprofloxacin Hydrochloride as an ophthalmic solution, the drug binds to bacterial DNA gyrase and topoisomeraseIV. This prevents DNA replication, leading to bacterial cell death. Because the molecule is lipophilic, it crosses the corneal epithelium quickly, achieving therapeutic levels in the aqueous humor within minutes. The typical regimen is one drop every two hours for the first 48hours, then four times daily for another five days.
Key Alternatives and Their Profiles
Below is a snapshot of the most frequently prescribed antibiotic eye drops that compete with Ciloxan. The table focuses on three dimensions that matter to clinicians and patients alike: spectrum of activity, dosing convenience, and known resistance trends (based on 2024‑2025 surveillance data from the US CDC and European Antimicrobial Resistance Network).
| Drug (Brand) | Active Ingredient & Strength | Spectrum (Gram‑±) | Typical Dosing | Resistance Concerns | Cost (US$ per bottle) |
|---|---|---|---|---|---|
| Ciloxan | Ciprofloxacin0.3% | Broad‑Gram‑+, Gram‑‑ (Pseudomonas) | Q2‑h → 4×/day | Increasing fluoroquinolone resistance in Staphaureus | 12-15 |
| Vigamox | Moxifloxacin0.5% | Broad‑Gram‑+, Gram‑‑ (including MRSA) | Q2‑h → 2×/day | Low resistance; expensive | 20-25 |
| Ocuflox | Ofloxacin0.3% | Broad‑Gram‑+, Gram‑‑ | Q2‑h → 4×/day | Similar to ciprofloxacin | 10-13 |
| Tobrex | Tobramycin0.3% | Gram‑‑ (Pseudomonas), limited Gram‑+ | Q2‑h → 4×/day | Low resistance in Pseudomonas, higher in Staph | 8-11 |
| Azyter | Azithromycin1% | Gram‑+, limited Gram‑‑ | Once daily | Very low resistance; good for mild cases | 15-18 |
| Genteal | Gentamicin0.3% | Gram‑‑, limited Gram‑+ | Q2‑h → 4×/day | Resistance rising in Pseudomonas | 9-12 |
When Ciloxan Is the Right Choice
- Severe bacterial keratitis: Fluoroquinolones achieve higher intra‑ocular concentrations, crucial for deep stromal infections.
- Known Pseudomonas involvement: Ciprofloxacin retains activity where many other agents falter.
- Patients needing rapid bactericidal action: The drug’s concentration‑dependent killing is faster than aminoglycosides.
- Cost‑sensitive settings: Ciloxan is cheaper than moxifloxacin while offering comparable coverage.
If the infection is mild, the patient is a child, or adherence is a concern, you might opt for a once‑daily alternative like azithromycin. Moreover, if local antibiograms show high fluoroquinolone resistance, a switch to tobramycin or gentamicin could be justified.
Safety and Tolerability Differences
All ophthalmic antibiotics can cause transient stinging, blurred vision, or allergic reactions. Fluoroquinolones (Ciloxan, Vigamox, Ocuflox) occasionally produce a temporary corneal epithelial defect in patients with pre‑existing dry eye. Aminoglycosides (tobramycin, gentamicin) have a higher risk of nephrotoxicity if systemic absorption occurs, though this is rare with standard eye‑drop dosing. Azithromycin is generally well‑tolerated, with the main complaint being a mild taste sensation.
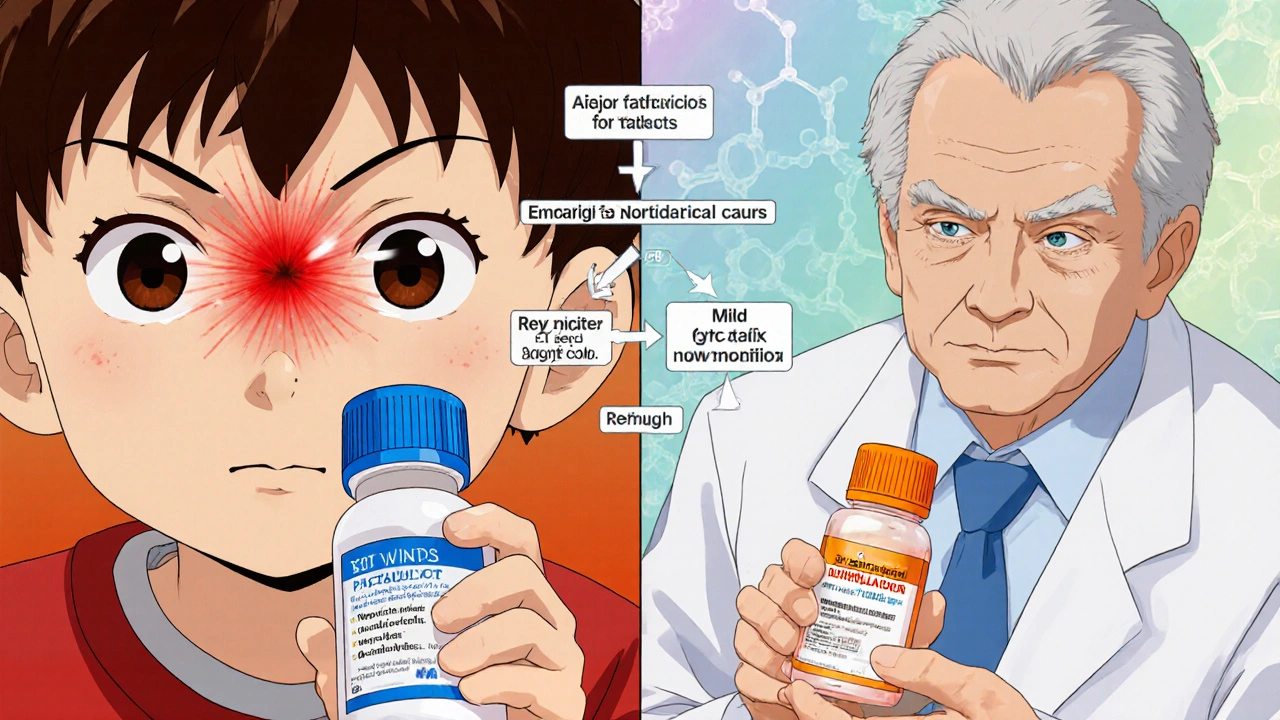
Practical Decision Tree for Clinicians
- Assess infection severity: Severe (keratitis, ulcer) → fluoroquinolone (Ciloxan or moxifloxacin).
- Check local resistance data: If >20% fluoroquinolone resistance, consider tobramycin or gentamicin.
- Evaluate patient factors: Pediatric patients may need gentamicin (lower pH); patients with compliance issues benefit from once‑daily azithromycin.
- Consider cost and insurance coverage: Ciloxan is often the most affordable broad‑spectrum option.
- Finalize choice and schedule follow‑up: Re‑examine after 48hours; switch if no improvement.
Common Pitfalls and How to Avoid Them
- Over‑reliance on a single drug: Rotate agents if a patient has recurrent infections to prevent resistance buildup.
- Ignoring allergies: Document any history of quinolone hypersensitivity before prescribing Ciloxan.
- Improper storage: Eye drops should be kept at room temperature and discarded after 28days once opened.
- Insufficient dosing: Patients often miss the “every‑two‑hours” phase; emphasize the importance of early intensive dosing.
Bottom Line: Matching the Drug to the Situation
In a nutshell, Ciloxan remains a solid first‑line option for most bacterial eye infections because of its broad coverage, proven efficacy, and affordable price. However, when resistance patterns shift, patient adherence is a concern, or the infection is mild, alternatives like moxifloxacin, azithromycin, or tobramycin can provide a better fit.
Frequently Asked Questions
Can I use Ciloxan for viral conjunctivitis?
No. Ciloxan targets bacteria; viral infections need antiviral agents or supportive care. Using an antibiotic won’t speed recovery and may foster resistance.
How long does it take for symptoms to improve?
Most patients notice reduced redness and discharge within 24-48hours of starting the intensive dosing phase. Full resolution usually occurs by day7.
Is it safe to use Ciloxan during pregnancy?
Animal studies have not shown teratogenic effects, but human data are limited. Discuss any eye‑drop use with your OB‑GYN; many clinicians prefer a safer alternative such as azithromycin if treatment is needed.
What should I do if I miss a dose?
Take the missed drop as soon as you remember, then resume the regular schedule. If it’s almost time for the next dose, skip the missed one-don’t double‑dose.
Are there any drug interactions with Ciloxan?
Topical ciprofloxacin has minimal systemic absorption, so interactions are rare. However, avoid using other topical ophthalmic medications within 5minutes to prevent dilution.





Write a comment
Your email address will be restricted to us