Fluoroquinolone Tendon Risk Calculator
Tendon Rupture Risk Assessment
This tool estimates your relative risk of tendon rupture while taking fluoroquinolone antibiotics based on your health factors. It's not a medical diagnosis, but can help you discuss risks with your doctor.
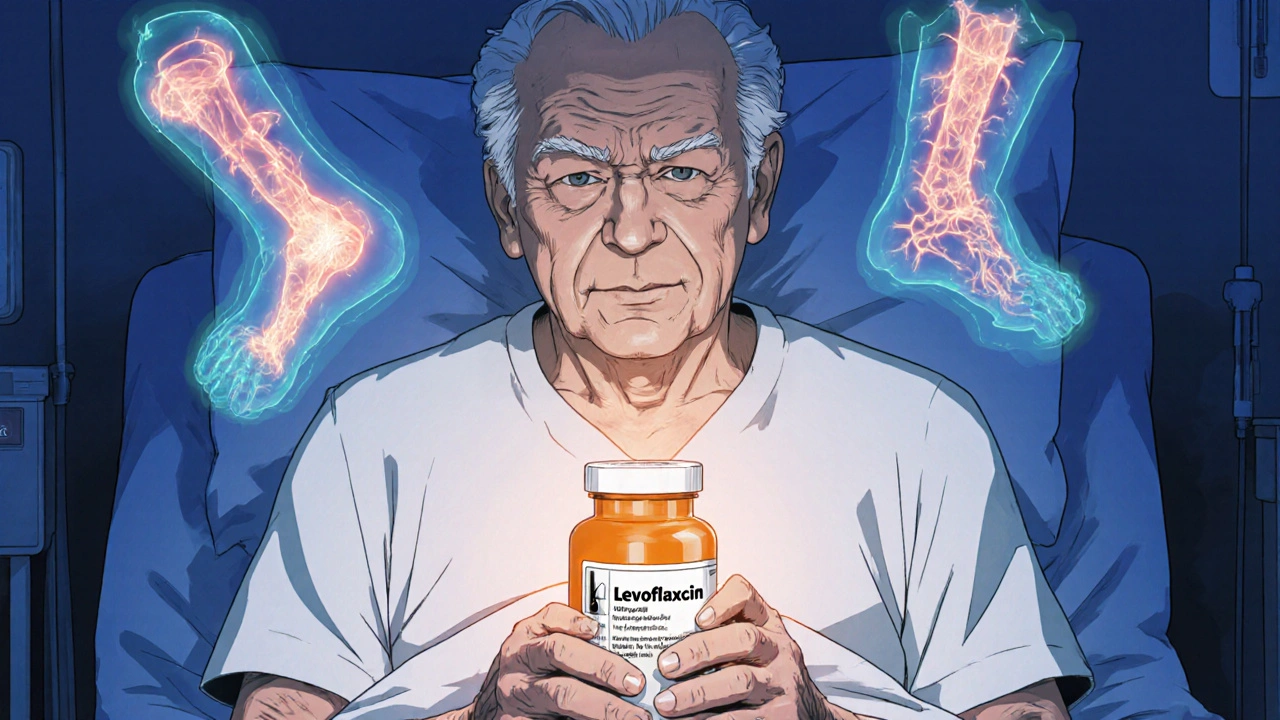
When you take an antibiotic like ciprofloxacin or levofloxacin for a stubborn infection, you expect relief-not a sudden, sharp pain in your heel that makes it impossible to walk. Yet for some people, these widely used antibiotics can trigger something far more serious than a stomach upset: tendon rupture. The risk isn’t rare. It’s real. And it’s growing in the medical community’s awareness.
Why Fluoroquinolones Are Still Prescribed
Fluoroquinolones, including drugs like ciprofloxacin, levofloxacin, and moxifloxacin, are powerful antibiotics. They’re used for serious infections that don’t respond to simpler treatments-complicated urinary tract infections, pneumonia, anthrax exposure, and certain types of abdominal infections. They work fast. They’re broad-spectrum. And for decades, doctors relied on them as go-to options. But here’s the catch: these antibiotics don’t just kill bacteria. They also interfere with how your body repairs and maintains connective tissue. That’s where the danger lies.The Achilles Tendon Is Most at Risk
If you’re taking a fluoroquinolone and start feeling pain, stiffness, or swelling in your ankle, don’t brush it off. The Achilles tendon-the thick band connecting your calf muscle to your heel-is the most vulnerable. Studies show it’s involved in nearly 90% of fluoroquinolone-related tendon injuries. In about half of those cases, both tendons are affected. It’s not just athletes or older adults. Even people who’ve never had a sports injury can develop tendon pain after just a few days on these drugs. One study found that 85% of cases show symptoms within the first month of starting treatment. Some patients report pain as early as two hours after taking their first pill.How the Damage Happens
Fluoroquinolones don’t just cause inflammation. They trigger cellular changes deep inside the tendon. Research suggests they:- Trigger cell death (apoptosis) in tendon cells
- Disrupt mitochondrial function, reducing energy production needed for tissue repair
- Interfere with collagen structure by binding to magnesium and calcium-minerals essential for tendon strength
- Stimulate the release of enzymes and free radicals that break down tendon tissue
Who’s at the Highest Risk?
Not everyone who takes fluoroquinolones will have problems. But certain people face dramatically higher odds:- Age 60 and older: Risk jumps 6-fold between 60-79, and more than 20-fold for those 80+
- Corticosteroid users: Taking prednisone or other steroids with a fluoroquinolone increases rupture risk by 46 times
- People with kidney disease: Impaired clearance means the drug stays in the body longer
- Diabetics: Poor blood flow and nerve damage make tendons more fragile
- Organ transplant recipients: Often on multiple drugs, including steroids
- Those with prior tendon injuries: Once damaged, tendons are more likely to fail again
The Corticosteroid Danger Zone
This is one of the most dangerous combinations in modern medicine. Taking a fluoroquinolone while on oral or injected steroids-common for conditions like asthma, arthritis, or autoimmune diseases-is like setting a fuse to a firework. The FDA and UK’s MHRA both warn against this combo. Yet, it still happens. Doctors sometimes don’t realize the patient is on a steroid. Patients don’t always mention it. And the result? A tendon that’s already weakened by steroids gets hit with a chemical that breaks down its structure. If you’re on prednisone or any steroid, fluoroquinolones should be avoided unless there’s no other option-and even then, you need to be monitored closely.When Symptoms Show Up-and When They Don’t
One of the scariest things about fluoroquinolone-induced tendinopathy is how unpredictable it is. Symptoms can appear:- As early as 48 hours after starting the drug
- After several weeks of treatment
- Or even weeks after you’ve finished the course
Regulatory Warnings and Global Changes
The risks aren’t hidden. They’ve been known for years. - The U.S. FDA added a black-box warning in 2008-the strongest possible alert-for tendon rupture and tendinitis. - In 2013 and again in 2018, the FDA expanded that warning to include disabling and potentially permanent side effects. - The UK’s MHRA restricted fluoroquinolones in 2019 to only the most serious infections where no other antibiotic works. - The European Medicines Agency (EMA) followed suit in 2018. These aren’t bureaucratic footnotes. They’re life-saving guidelines. Today, the Infectious Diseases Society of America (IDSA) recommends fluoroquinolones be used as a last resort for common infections like sinusitis, bronchitis, or uncomplicated UTIs.What to Do If You’re Prescribed a Fluoroquinolone
If your doctor suggests a fluoroquinolone, ask:- Is this the only option?
- Have you considered alternatives like amoxicillin, doxycycline, or trimethoprim-sulfamethoxazole?
- Am I on any steroids or other drugs that increase my risk?
- What signs should I watch for?
What Happens After a Tendon Rupture?
A ruptured tendon doesn’t heal on its own. It usually requires surgery, followed by months of physical therapy. Even then, full strength and mobility may never return. Some patients end up with chronic pain, limping, or the need for assistive devices. And recovery isn’t just physical. The psychological toll is real. People who’ve had a rupture report anxiety about movement, fear of reinjury, and loss of independence.Why This Isn’t Just an ‘Old People’ Problem
It’s easy to think, “I’m young and fit-I’m fine.” But tendon damage from fluoroquinolones doesn’t care about fitness level. A 38-year-old marathon runner was documented in a case report to rupture their Achilles tendon after a 7-day course of levofloxacin for a urinary infection. The problem isn’t age. It’s biology. And if your body’s tendon repair system is already under stress-whether from diabetes, steroid use, or even just a minor prior injury-you’re more vulnerable.What’s Being Done to Fix This?
Researchers are now looking at:- Genetic markers that might predict who’s at higher risk
- Whether certain fluoroquinolones are safer than others (moxifloxacin may carry lower risk than levofloxacin, but data is mixed)
- Drug modifications to reduce tendon toxicity while keeping antibacterial power
Final Takeaway
Fluoroquinolones save lives. But they also carry a hidden cost. For many, that cost is a ruptured tendon-and the life-altering recovery that follows. Don’t let convenience override caution. If your doctor reaches for a fluoroquinolone, ask why. Push for alternatives. Know the warning signs. And if you feel pain in your tendons-no matter how mild-act fast. It’s not just a side effect. It’s a warning sign your body can’t afford to ignore.Can fluoroquinolones cause tendon rupture even after I stop taking them?
Yes. While most tendon issues appear during treatment, symptoms can develop weeks or even months after stopping the antibiotic. The FDA and MHRA both warn that tendon damage can occur after discontinuation. If you feel sudden pain, swelling, or stiffness in a tendon-even months later-seek medical advice immediately.
Are all fluoroquinolones equally risky?
No. Levofloxacin and ciprofloxacin are most commonly linked to tendon rupture, making up about 88% of reported cases. Moxifloxacin is involved less often, but still carries risk. No fluoroquinolone is considered safe for people with known risk factors like age over 60 or steroid use. The entire class has been flagged by regulators.
Is it safe to take fluoroquinolones if I’m healthy and under 60?
Even if you’re young and healthy, fluoroquinolones should be reserved for serious infections where safer antibiotics won’t work. For common issues like sinus infections, bronchitis, or uncomplicated UTIs, there are usually better, safer options. The risk is low for healthy people-but it’s not zero. Always ask if alternatives exist.
What should I do if I experience tendon pain while on a fluoroquinolone?
Stop taking the antibiotic immediately. Contact your doctor right away. Avoid putting weight on the affected area. Do not stretch or massage the tendon. Your doctor will likely recommend imaging (like an ultrasound or MRI) and may refer you to a specialist. Early intervention can prevent a full rupture.
Why do some studies say fluoroquinolones don’t increase tendon rupture risk?
Some studies, particularly smaller or region-specific ones, have found no clear link. For example, a 2022 Japanese study using a unique control method didn’t find a significant association. But these are outliers. Large-scale analyses from the UK, Taiwan, and the U.S., involving millions of patients, consistently show elevated risk. Regulatory agencies worldwide have acted based on the overwhelming body of evidence-not single studies.



Write a comment
Your email address will be restricted to us