One glass of grapefruit juice in the morning might seem like a healthy start - but if you're taking certain medications, it could be dangerous. This isn't a myth or a warning from an old wives’ tale. It’s a well-documented, clinically proven interaction that can send you to the hospital - or worse. Since the 1989 discovery by Canadian researchers, we’ve learned that grapefruit juice doesn’t just affect how your body processes a few drugs. It can change how your entire system handles dozens of common prescriptions, sometimes with life-threatening results.
Why Grapefruit Juice Changes How Your Medicines Work
Grapefruit juice doesn’t interact with medications because it’s acidic or sugary. It’s because of chemicals called furanocoumarins, mainly bergamottin and 6',7'-dihydroxybergamottin. These compounds shut down an enzyme in your gut called CYP3A4. That enzyme is responsible for breaking down about half of all oral medications before they enter your bloodstream. When it’s blocked, your body absorbs way more of the drug than it should.
Think of it like this: your body is designed to let in just the right amount of a drug. Grapefruit juice removes the safety valve. That means if you take a statin like simvastatin with grapefruit juice, you might get three times the intended dose. That’s not a little extra benefit - that’s a spike into toxic territory. And the worst part? One glass is enough. A 200-milliliter serving (about 6.7 ounces) can block CYP3A4 by nearly 50% within four hours. That effect lasts up to 72 hours. So even if you drink grapefruit juice at breakfast and take your pill at night, you’re still at risk.
Which Medications Are Most at Risk?
More than 85 medications are known to interact with grapefruit juice. But not all are equally dangerous. The FDA and other health agencies have flagged the most critical ones based on real-world outcomes. Here are the big ones:
- Statins - These cholesterol-lowering drugs are the most common offenders. Simvastatin (Zocor) is especially risky. Just one glass of grapefruit juice a day for three days can triple its concentration in your blood. That dramatically increases your risk of rhabdomyolysis - a condition where muscle tissue breaks down, which can lead to kidney failure. Atorvastatin (Lipitor) has a smaller interaction, while pravastatin and rosuvastatin are safe. If you’re on simvastatin, switching to one of these alternatives is a smart move.
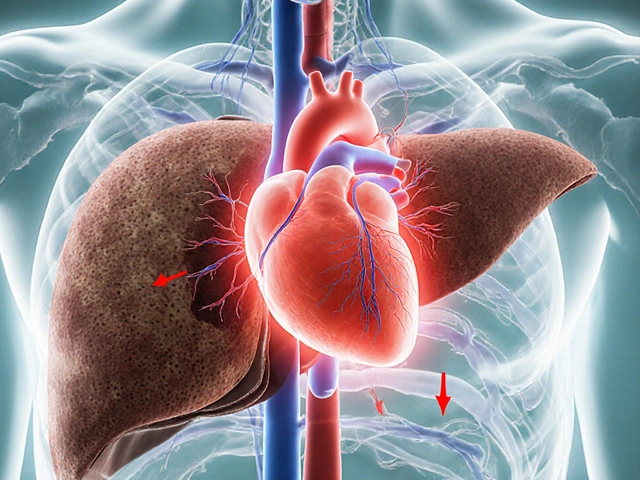
- Calcium channel blockers - Used for high blood pressure and chest pain. Felodipine (Plendil) can see a fivefold increase in blood levels. Nifedipine (Procardia) jumps by 3.3 times. But amlodipine (Norvasc)? Minimal effect. If you’re on one of these, your doctor should know which one you’re taking - because not all are created equal.
- Immunosuppressants - Drugs like cyclosporine (Neoral) and tacrolimus are used after organ transplants. Grapefruit juice can push cyclosporine levels up by 50-60%. That raises the risk of kidney damage. Patients on these drugs often need strict dietary rules - and grapefruit is almost always off-limits.
- Antiarrhythmics - Amiodarone (Cordarone), used for irregular heartbeats, can see a 30-40% increase in blood concentration with grapefruit. That can trigger dangerous heart rhythms.
- Other high-risk drugs - Some antidepressants, anti-anxiety meds, and even certain cancer drugs like docetaxel and erlotinib are affected. Always check your prescription label.
On the flip side, some drugs show little to no interaction. Trazodone (for sleep and depression) and zolpidem (Ambien) are generally safe. But here’s the catch: you can’t assume. Unless your doctor or pharmacist confirms it’s safe, don’t risk it.
Not All Citrus Is the Same
Just because you’re avoiding grapefruit doesn’t mean you can freely drink orange juice. Seville oranges - the kind used in marmalade - contain the same furanocoumarins. Pomelos, a larger cousin of grapefruit, are just as risky. But sweet oranges (like Valencia or navel) and lemons? They’re fine. They don’t have those harmful compounds. So if you’re craving citrus, stick to those. But don’t assume all orange-flavored drinks are safe - some artificial flavors are made from Seville orange extracts. Read labels.

Why This Isn’t Just About Timing
You might think, “I’ll just take my pill two hours after my grapefruit juice.” That won’t work. Unlike most drug interactions - where timing matters - grapefruit juice causes permanent damage to the CYP3A4 enzyme in your gut. Your body has to grow new enzymes to replace them. That takes one to three days. So even if you drink grapefruit juice on Monday and take your pill on Wednesday, you’re still at risk. The FDA says it clearly: “Avoid grapefruit the whole period you are on the medication.” Not just at dosing time. Not just when you drink it. All the time.
Who’s Most at Risk?
Older adults are the most vulnerable group. People over 65 make up 40% of grapefruit juice consumers in the U.S., according to USDA data. And they’re also the ones most likely to be taking three to five medications at once - many of which interact with grapefruit. A 72-year-old on simvastatin, a calcium channel blocker, and a blood thinner? That’s a perfect storm. Even small amounts of grapefruit juice can push drug levels into danger zones.
Genetics also play a role. Some people naturally have more CYP3A4 enzyme in their gut. For them, grapefruit juice causes a much bigger spike in drug levels. Others have less enzyme - so the effect is smaller. But there’s no test to tell you which group you’re in. So everyone on affected medications needs to assume they’re in the high-risk group.
What Should You Do?
Here’s what works in real life:
- Check every prescription. Look at the patient information leaflet. If it says “avoid grapefruit,” take it seriously. If it doesn’t mention grapefruit, ask your pharmacist anyway. Not all labels are updated, and not all providers know the latest data.
- Make a list. Write down every medication you take - including over-the-counter drugs, supplements, and herbal products. Some supplements like St. John’s Wort also affect CYP3A4. Bring this list to every doctor visit.
- Ask your pharmacist. Pharmacists are trained to catch these interactions. A 2021 study found 89% of community pharmacists routinely screen for grapefruit interactions when filling prescriptions. Don’t skip this step.
- Ask about alternatives. If you’re on simvastatin and love grapefruit, ask if you can switch to pravastatin or rosuvastatin. If you’re on felodipine, maybe amlodipine is a better fit. These switches are common and often covered by insurance.
- Don’t guess. If you’re unsure, skip it. There’s no benefit to taking the risk. The consequences - muscle damage, kidney failure, heart rhythm problems - are not worth it.

The Bigger Picture: Why This Keeps Happening
Despite decades of warnings, patient awareness is still low. A 2022 survey found only 38% of patients recalled being told about grapefruit interactions when they were prescribed affected drugs. That’s not because doctors are careless. It’s because there are so many drugs, so many interactions, and so little time in appointments. The FDA now requires drugmakers to test new oral medications for grapefruit interactions during development. But that doesn’t help people already on old prescriptions.
Some companies are trying to fix this. In October 2023, the USDA announced CRISPR-edited grapefruit with 90% less furanocoumarin had passed early safety trials. If this becomes available, it could change everything. But for now, the only safe option is to avoid it entirely.
What If You Accidentally Ate Some?
If you had a glass of grapefruit juice and later realized you’re on a risky medication, don’t panic. But do act. Skip your next dose if you’re unsure. Call your doctor or pharmacist. Tell them exactly what you consumed and when. They can check your drug levels if needed - especially for drugs like cyclosporine or amiodarone where toxicity can be life-threatening. In most cases, one accidental exposure won’t cause harm. But repeated use? That’s how emergencies happen.
Final Advice: When in Doubt, Skip It
Grapefruit juice isn’t evil. It’s full of vitamin C and antioxidants. But when it comes to medications, it’s a silent danger. You can’t see it, taste it, or feel it until it’s too late. The safest choice isn’t complicated: if you’re on a medication that interacts with grapefruit, don’t drink it. Ever. Not even once. Not even if you think you’re fine. Not even if your friend drinks it with their pills. Your body is different. Your meds are different. The risk is real.
There are plenty of other healthy drinks. Water. Green tea. Lemon water. Apple juice. You don’t need grapefruit to be healthy. But you do need to be safe.
Can I drink grapefruit juice if I take my medication at night?
No. Grapefruit juice blocks the CYP3A4 enzyme in your gut, and the effect lasts 24 to 72 hours. Even if you drink it in the morning and take your pill at night, the enzyme is still blocked. The interaction isn’t about timing - it’s about whether the enzyme is active when your drug passes through your gut. Avoid grapefruit juice entirely while on affected medications.
Is orange juice safe to drink with medications?
Sweet oranges - like navel or Valencia - are safe. They don’t contain furanocoumarins. But Seville oranges (used in marmalade) and pomelos are just as dangerous as grapefruit. Always check the label. Some orange-flavored drinks may contain Seville orange extract, so read ingredients carefully.
Do all statins interact with grapefruit juice?
No. Simvastatin has the strongest interaction - one glass can triple its levels. Atorvastatin has a mild interaction. Pravastatin and rosuvastatin show no significant interaction. If you’re on simvastatin and enjoy grapefruit, talk to your doctor about switching. The change is often simple and covered by insurance.
Can grapefruit juice affect over-the-counter drugs?
Yes. Some OTC medications, like certain antihistamines (e.g., fexofenadine/Allegra), can be affected. Even some herbal supplements like St. John’s Wort interact with grapefruit. Always check the label or ask your pharmacist before combining anything with grapefruit juice.
Why do some people say they drink grapefruit juice with their meds and are fine?
Because everyone’s body is different. Some people have less CYP3A4 enzyme naturally, so the interaction is weaker. Others have more - and get dangerously high drug levels. You can’t tell which group you’re in without genetic testing, which isn’t done in routine care. So even if someone else seems fine, it doesn’t mean it’s safe for you. The safest rule is to avoid it completely.




Write a comment
Your email address will be restricted to us