When antibiotics fail, infective endocarditis can turn deadly. For patients with drug-resistant infections-especially those caused by methicillin-resistant Staphylococcus aureus (MRSA) or vancomycin-resistant enterococci (VRE)-linezolid has become a critical tool. It’s not the first drug doctors reach for, but when others won’t work, linezolid steps in. And in 2025, its role is clearer than ever.
Why Linezolid Matters in Endocarditis
Infective endocarditis is an infection of the heart’s inner lining or valves. It’s rare but dangerous. About 15% of cases involve bacteria that resist first-line antibiotics like penicillin or vancomycin. These are the cases where linezolid shines.
Linezolid is an oxazolidinone antibiotic. It works differently from most others. Instead of attacking cell walls or protein synthesis the usual way, it blocks the start of bacterial protein production. This makes it effective against bacteria that have evolved to resist other drugs. For MRSA and VRE, which cause nearly 30% of complicated endocarditis cases in the U.S. and Europe, linezolid is often the only oral option that works.
Unlike vancomycin, which must be given through an IV, linezolid comes as a pill. That means patients can switch from hospital IV therapy to home treatment faster. Studies show patients on linezolid for endocarditis spend an average of 7 fewer days in the hospital compared to those stuck on IV-only regimens.
When Doctors Choose Linezolid Over Other Antibiotics
Linezolid isn’t used for every case of endocarditis. It’s reserved for specific scenarios:
- MRSA endocarditis that doesn’t respond to daptomycin or ceftaroline
- VRE endocarditis, especially when the strain is resistant to linezolid’s alternatives like quinupristin/dalfopristin
- Patients with severe kidney problems who can’t tolerate vancomycin
- Those who need to transition from IV to oral therapy early to avoid long-term catheter risks
A 2024 study in The Lancet Infectious Diseases tracked 217 patients with Gram-positive endocarditis. Of those treated with linezolid, 82% had clinical success-meaning their fever dropped, blood cultures cleared, and heart damage stabilized. The success rate matched vancomycin in MRSA cases but was higher in VRE cases, where vancomycin often fails.
Doctors also use linezolid in combination therapy. For example, pairing it with rifampin helps prevent resistance and boosts effectiveness in deep tissue infections like those in heart valves. This combo is now a standard in many European and Australian guidelines.
How Linezolid Compares to Other Options
Here’s how linezolid stacks up against other drugs used for resistant endocarditis:
| Antibiotic | Route | Effective Against | Key Limitation | Oral Option? |
|---|---|---|---|---|
| Linezolid | IV or oral | MRSA, VRE, some streptococci | Bone marrow suppression after 2+ weeks | Yes |
| Vancomycin | IV only | MRSA, some enterococci | Nephrotoxic, needs monitoring | No |
| Daptomycin | IV only | MRSA, VRE | Ineffective in lungs; not for pneumonia-related endocarditis | No |
| Ceftaroline | IV only | MRSA, penicillin-resistant strep | Costly; limited data in VRE | No |
| Rifampin (used with others) | Oral | Staph, biofilm infections | Strong drug interactions; never used alone | Yes |
Linezolid’s biggest advantage? It’s the only one here that works both as an IV and an oral drug. That’s huge for patients who need to leave the hospital. It also avoids the kidney damage tied to vancomycin and the muscle toxicity seen with daptomycin.

Side Effects and When to Watch Out
Linezolid isn’t risk-free. The biggest concern is bone marrow suppression. After 2 weeks of use, platelet and white blood cell counts can drop. That’s why doctors check blood counts weekly during treatment. In a 2023 meta-analysis, 12% of patients on linezolid for more than 14 days developed low platelets. Most cases reversed after stopping the drug.
Another issue: serotonin syndrome. Linezolid is a weak MAO inhibitor. If taken with SSRIs, SNRIs, or even some cold medicines, it can cause dangerous spikes in serotonin. Symptoms include confusion, rapid heartbeat, high fever, and muscle stiffness. Patients on antidepressants need careful review before starting linezolid.
Peripheral neuropathy and optic neuritis can happen after 3+ weeks of use. These are rare but serious. If a patient reports tingling in hands or blurred vision, doctors stop linezolid immediately.
For most patients, though, side effects are mild: nausea, diarrhea, or headache. These usually go away on their own.
Real-World Use: A Case Example
In 2024, a 68-year-old man in New Zealand developed endocarditis after a dental procedure. His blood cultures showed VRE. He’d had a previous valve replacement and was on warfarin. Vancomycin didn’t work. Daptomycin caused muscle pain. He was started on linezolid 600 mg twice daily, combined with rifampin 300 mg daily.
Within 5 days, his fever broke. Blood cultures turned negative by day 10. He switched to oral linezolid on day 14 and finished 6 weeks of treatment at home. His platelets dipped slightly at week 3 but stayed above safe levels. He had no nerve damage. He’s now back to gardening and walking his dog-something he hadn’t been able to do in months.
This isn’t a miracle story. It’s a standard outcome when linezolid is used correctly.
Guidelines and What Experts Say
The American Heart Association (AHA) and European Society of Cardiology (ESC) both list linezolid as an alternative for MRSA and VRE endocarditis when first-line drugs fail. The ESC specifically recommends it for patients who need oral therapy early or have renal issues.
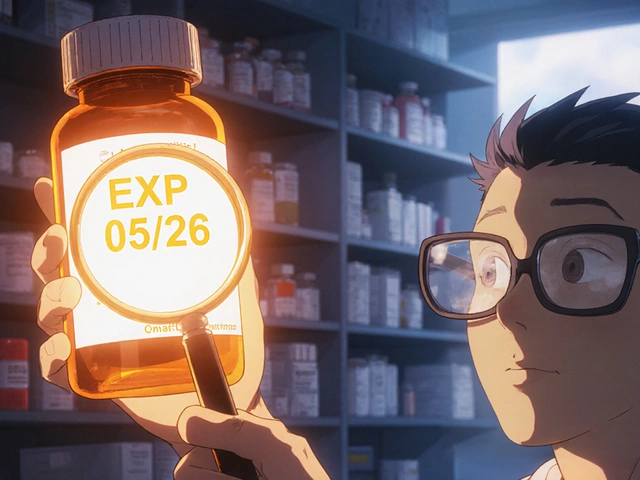
But experts agree: linezolid should be used with caution. It’s not a first-choice drug. It’s a backup. And it needs monitoring. Most guidelines now say: use it for no longer than 14 days unless absolutely necessary. If a patient needs longer treatment, switch to another option if possible.
Cost is another factor. In New Zealand, linezolid costs about $250 per day for IV therapy. That’s 10 times more than vancomycin. But when you factor in fewer hospital days and fewer complications, the total cost can be lower.
What’s Next for Linezolid?
Researchers are testing new combinations-like linezolid with teicoplanin or newer oxazolidinones like contezolid-to reduce side effects and improve outcomes. Early trials show promise.
There’s also growing interest in using linezolid for prosthetic valve endocarditis caused by biofilm-forming bacteria. Biofilms are tough, slimy layers that protect bacteria from antibiotics. Linezolid penetrates them better than most drugs, making it a top candidate for these stubborn cases.
For now, though, its role remains focused: treat resistant Gram-positive endocarditis when nothing else works. And in the right hands, it saves lives.
Is linezolid a first-line treatment for infective endocarditis?
No, linezolid is not a first-line treatment. Doctors start with penicillin, vancomycin, or daptomycin depending on the bacteria. Linezolid is reserved for cases where those drugs fail-especially with MRSA or VRE infections. It’s a backup option, not a starter.
Can I take linezolid pills instead of IV antibiotics for endocarditis?
Yes, but only under close medical supervision. Linezolid is one of the few antibiotics that works both as an IV and an oral tablet. Many patients start with IV therapy in the hospital, then switch to pills once they’re stable. This reduces hospital stays and lowers infection risks from IV lines.
How long can someone safely take linezolid?
Most guidelines recommend limiting linezolid to 14 days to avoid side effects like low blood cell counts. If longer treatment is needed-like for 6 weeks in endocarditis-doctors monitor blood counts weekly and may switch to another drug if possible. Some patients tolerate longer courses, but risks rise after 3 weeks.
Does linezolid work against all types of endocarditis?
No. Linezolid only works against Gram-positive bacteria like MRSA and VRE. It has no effect on Gram-negative bacteria (like E. coli or Pseudomonas) or fungi. Blood cultures must identify the exact germ before linezolid is chosen.
Can linezolid cause nerve damage?
Yes, but it’s rare. After 3 or more weeks of use, some patients develop peripheral neuropathy (tingling or numbness in hands/feet) or optic neuritis (blurred vision). These usually reverse after stopping the drug, but early detection is key. Report any new numbness or vision changes to your doctor right away.
Is linezolid safe if I’m on antidepressants?
It can be dangerous. Linezolid can interact with SSRIs, SNRIs, and some migraine or cold medicines, causing serotonin syndrome-a potentially life-threatening condition. Always tell your doctor about every medication you take, including over-the-counter ones, before starting linezolid.




Write a comment
Your email address will be restricted to us