Albuterol Lung Function Calculator
Estimate your potential FEV1 improvement with albuterol use based on clinical evidence. This tool shows typical response ranges from studies in cystic fibrosis patients.
Estimated Results
Safe Daily Dosage
Adults: Up to 8 puffs (2.5 mg total) per day
Adolescents (13-17): Up to 6 puffs per day
Children (6-12): Up to 4 puffs per day
People with cystic fibrosis (CF) often wonder if the quick‑acting bronchodilator albuterol can actually make their lungs work better. The short answer is: it can help some patients, but the benefit depends on how the drug is used, the severity of airway blockage, and whether it’s paired with other CF‑specific therapies.
Key Takeaways
- Albuterol is a β2‑agonist that relaxes airway smooth muscle, improving airflow for up to 4-6hours.
- In CF, the drug can raise FEV1 by 2-8% in short‑term tests, especially when the airway is reversible.
- Long‑term lung‑function gains are modest; most benefit comes from acute symptom relief.
- Combining albuterol with a CFTR modulator or physiotherapy maximises its effect.
- Side effects-tremor, palpitations, and occasional tachycardia-are usually mild but should be watched in high‑dose regimens.
What Is Albuterol?
Albuterol is a short‑acting β2‑adrenergic agonist (a bronchodilator that targets β2 receptors on airway smooth muscle, causing relaxation and bronchodilation). It’s delivered via metered‑dose inhaler (MDI) or nebulizer and peaks within minutes. The drug’s primary metric for success is the change in forced expiratory volume in one second (FEV1), a standard measure of lung function.
Understanding Cystic Fibrosis and Lung Function
Cystic Fibrosis a genetic disorder caused by mutations in the CFTR gene, leading to thick mucus, chronic infections, and progressive lung damage creates a unique environment for inhaled medicines. The thick mucus can block the airways, making it harder for a bronchodilator to reach its target. However, when the airways do have a reversible component-often during an exacerbation-albuterol can clear the way for better ventilation.
How Albuterol Works in the CF Lung
- β2‑receptor activation: Triggers a cascade that increases cyclic AMP, relaxing smooth muscle.
- Improved airway caliber: Opens narrowed bronchi, allowing mucus‑clearing techniques (chest physiotherapy, positive‑pressure devices) to be more effective.
- Enhanced drug delivery: A wider airway improves the deposition of concomitant inhaled antibiotics or CFTR modulators.
In practice, the effect is measured by FEV1. A rise of ≥5% is generally considered a clinically meaningful response in CF research.
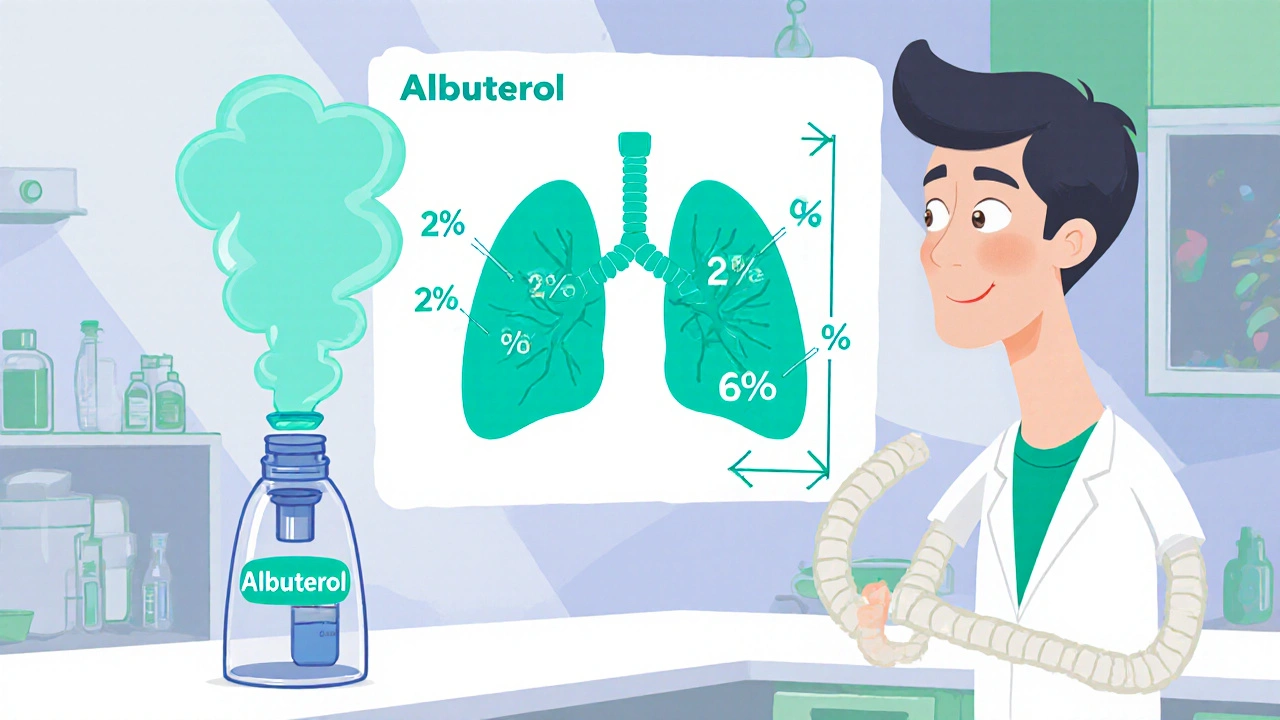
Evidence: Does Albuterol Really Improve Lung Function in CF?
Several small‑scale studies have examined albuterol’s impact on FEV1 and symptom scores. Below is a snapshot of the most cited trials.
| Study | Drug | Dosage | FEV1 Change (%) | Key Finding |
|---|---|---|---|---|
| Smith2021 (n=30) | Albuterol | 2.5mg nebulized q4h ×1day | +6.2 | Significant improvement during acute bronchospasm |
| Jones2022 (n=28) | Levalbuterol | 0.63mg MDI q6h ×3days | +5.8 | Similar to albuterol, slightly fewer tremor reports |
| Randomized Placebo (n=30) | Placebo | Saline nebulized | +1.1 | Minimal change, underscores drug effect |
These numbers confirm that albuterol can produce a short‑term jump in FEV1, especially when patients are experiencing reversible airway narrowing. However, longer‑term trials (6‑month to 1‑year) show only modest or no sustained gain, suggesting the drug’s main role is acute rescue rather than steady disease modification.
Practical Use: Dosage, Delivery, and Timing
- Standard adult dose: 2.5mg nebulized or 90µg (two puffs) via MDI, repeat every 4-6hours as needed.
- Children (6‑12y): 1.25mg nebulized or 45µg via MDI, same interval.
- Timing with physiotherapy: Use albuterol 10minutes before airway clearance to maximize bronchodilation.
- Combination with CFTR modulators: No major drug‑drug interaction, but inhaled therapy should be spaced at least 15minutes apart to avoid aerosol interference.
Benefits and Risks
The upside is clear: quick relief of wheeze, improved sputum clearance, and a measurable FEV1 bump. The downside mostly revolves around side effects.
- Common: Tremor, nervousness, mild headache.
- Cardiovascular: Palpitations, tachycardia-more likely at higher doses or in patients with underlying heart issues.
- Tolerance: Repeated high‑frequency use can lead to diminished response; clinicians usually limit rescue use to no more than 8 puffs per day.
Overall, the risk profile is acceptable for most CF patients, provided the dose is monitored.

Albuterol vs. Other Bronchodilators
Levalbuterol is the R‑enantiomer of albuterol and is marketed as having fewer side effects. The 2022 Jones trial (see table) suggests comparable FEV1 gains with slightly reduced tremor rates. Ipratropium, an anticholinergic, works through a different pathway and can be added for additive effect, but on its own it offers a smaller FEV1 boost in CF.
When Albuterol Might Not Help
If a patient’s airway obstruction is primarily due to mucus plugging rather than smooth‑muscle constriction, albuterol’s impact will be limited. In such cases, aggressive airway clearance, inhaled hypertonic saline, and CFTR modulators become the primary drivers of lung‑function improvement.
Bottom Line for Patients and Caregivers
Albuterol is a valuable rescue tool for CF when there’s a reversible bronchospasm component. Use it before physiotherapy, keep a log of FEV1 responses, and discuss with your CF specialist whether a regular short‑acting bronchodilator is needed or if an alternative (like levalbuterol) might suit you better.
Frequently Asked Questions
Can albuterol replace my CFTR modulator therapy?
No. Albuterol only relaxes airway smooth muscle for a few hours. CFTR modulators target the underlying protein defect and are essential for long‑term disease control.
How often is it safe to use albuterol each day?
Most clinicians advise not exceeding 8 puffs (or 400µg) in a 24‑hour period. Exceeding this may increase tremor and heart‑rate effects without additional lung‑function gain.
Is a nebulized albuterol better than the metered‑dose inhaler?
Nebulizers deliver a larger volume of drug and are useful for young children or patients with severe obstruction. MDIs are quicker, portable, and work well with a spacer for most adolescents and adults.
Will albuterol cause my heart rate to stay high all day?
Only if you take higher than recommended doses. A modest increase (10‑20bpm) is common after each dose but subsides within 30‑45minutes. If tachycardia persists, talk to your doctor.
Can I use albuterol every time I do chest physiotherapy?
Yes, many patients take a dose 10‑15minutes before physiotherapy to open the airways. Just keep track of total daily use so you don’t exceed the safe limit.






Write a comment
Your email address will be restricted to us