Every year, millions of patients receive the wrong medication, wrong dose, or a drug that clashes with their other prescriptions. These aren’t hypothetical risks-they’re real, measurable, and happening right now in pharmacies across the world. In fact, a 2023 global review found that dispensing errors occur in about 1.6% of all prescriptions filled. That might sound small, but when you consider billions of prescriptions filled annually, it means hundreds of thousands of people are at risk. And behind every error is a patient who could be hurt-or worse.
What Are the Most Common Pharmacy Dispensing Errors?
Not all mistakes look the same. Some are obvious, like handing a patient insulin when they were prescribed metformin. Others are quieter but just as dangerous-like giving a patient the wrong strength of a blood thinner, or missing a life-threatening allergy because the label was too small to read. The top three errors, according to the Academy of Managed Care Pharmacy (2023), are:- Dispensing the wrong medication, strength, or form (32% of all errors)
- Miscalculating the dose (28%)
- Failing to catch dangerous drug interactions or contraindications (24%)
- Expired meds-medications stored improperly or not rotated properly on the shelf
- Wrong duration-giving a 30-day supply when the prescription says 7 days
- Incorrect preparation-compounding errors, like using the wrong diluent for IV antibiotics
- Wrong route-giving an oral tablet as if it were meant to be injected
Why Do These Errors Happen?
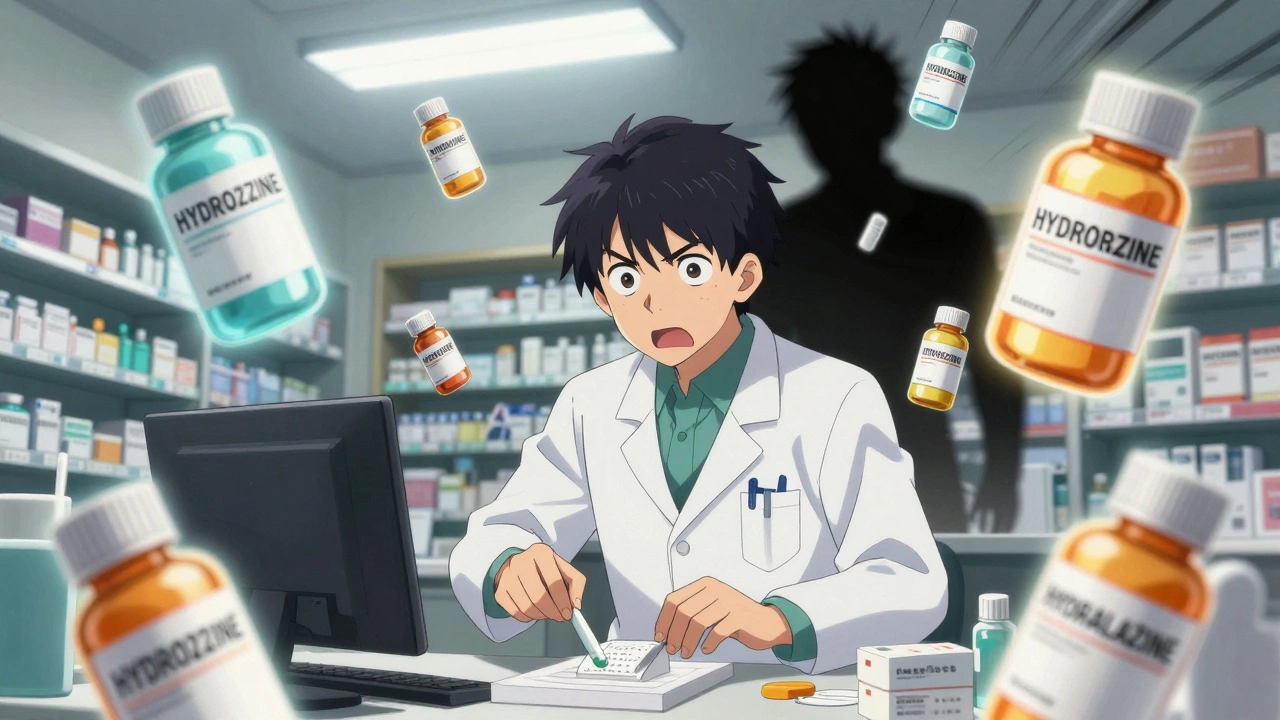
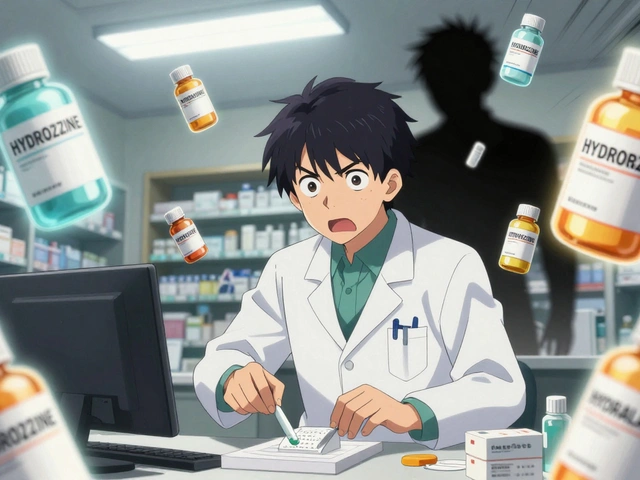
It’s easy to blame the pharmacist. But the truth? Most errors come from broken systems, not bad people. The biggest culprit? Workload. A 2023 analysis found that 37% of dispensing errors happen because pharmacists are rushed, understaffed, or juggling too many tasks at once. When you’re filling 80 prescriptions an hour, your brain starts taking shortcuts. And that’s when mistakes slip through. Another major issue? Similar-looking or sound-alike drug names. Think of hydroxyzine and hydralazine. One’s an antihistamine. The other’s a blood pressure drug. Mix them up, and you could send someone into cardiac arrest. Sound-alike names cause 22% of errors when prescriptions are called in. Handwritten prescriptions? They’re still around-and they’re responsible for 43% of errors because of illegible handwriting. Interruptions are just as dangerous. If a pharmacist is interrupted three or more times while filling a prescription, the chance of an error jumps by 12.7%. That’s not a coincidence. It’s how the human brain works. Focus breaks. Attention fades. Details get missed. And then there’s the lack of critical information. Nearly 30% of errors happen because the prescriber didn’t provide enough context-no lab values, no allergy history, no weight or kidney function data. Pharmacists can’t be mind readers. If the system doesn’t give them the full picture, they’re flying blind.How to Prevent Dispensing Errors: Proven Strategies
Preventing these errors isn’t about working harder. It’s about working smarter. Here’s what actually works:1. Double-Check High-Risk Medications
Certain drugs demand extra care. Insulin, heparin, opioids, and chemotherapy agents are on the “high-alert” list for a reason. One hospital reported a 78% drop in errors after requiring two pharmacists to independently verify every dose of insulin before it left the pharmacy. That’s not overkill-it’s necessary.2. Use Barcode Scanning
Barcodes aren’t just for groceries. When pharmacies scan both the prescription and the medication before dispensing, they cut errors by nearly half. A 2021-2023 survey of 127 hospitals found barcode systems reduced:- Wrong drug errors by 52.1%
- Wrong dose errors by 48.7%
- Wrong dosage form errors by 45.3%
3. Implement Tall Man Lettering
This simple fix changes how similar drugs are labeled. Instead of writing “HYDROXYZINE” and “HYDRALAZINE,” they’re printed as “HYDROXYZINE” and “HYDRALAZINE.” The capital letters highlight the difference. Pharmacies that adopted this saw a 56.8% drop in mix-ups. It costs nothing. It takes no training. It just works.4. Use Clinical Decision Support Tools
Modern pharmacy software doesn’t just fill prescriptions-it flags problems. If a patient is on warfarin and the prescriber orders ibuprofen, the system should scream: “Risk of bleeding!” If the patient has kidney disease and the dose isn’t adjusted, it should stop the process. Systems with these alerts reduce interaction errors by 53%. But there’s a catch: too many alerts cause “alert fatigue.” Pharmacists start ignoring them. The key? Smart, targeted alerts-not constant noise.5. Standardize Processes and Reduce Interruptions
Create a “no interruption zone” during high-risk tasks like preparing IV bags or checking anticoagulant doses. Use visual signals-like a red light or a sign-that say, “Do not disturb.” One pharmacy in Wellington reduced errors by 40% after installing these zones. Staff reported feeling less stressed. Patients felt safer.6. Improve Communication with Prescribers
If a prescription is unclear, call the doctor. Don’t guess. Don’t assume. Don’t fill it and hope for the best. A 2023 study found that pharmacies with direct, real-time access to prescribers reduced errors by 31%. Electronic prescribing (e-prescribing) helps, but even in places without it, a quick phone call beats a dangerous assumption.
Technology Isn’t the Whole Answer
You might think the answer is just more tech: robots, AI, automated dispensers. And yes, they help. Robotic systems have cut errors by 63% in some hospitals. AI tools predict potential errors before they happen, reducing mistakes by over 50% in pilot programs. But here’s the problem: technology introduces new risks. A 2023 study showed that while computerized prescribing cut errors by 43%, it created new ones in 17.8% of cases-like confusing drop-down menus or auto-filled wrong doses. One pharmacist on Reddit wrote: “Our new system auto-filled 500mg instead of 50mg because the default was wrong. We didn’t notice until the patient showed up with seizures.” Tech is a tool, not a fix. The real solution is a human-centered system: technology that supports, not replaces, careful judgment.What Patients Can Do
You don’t have to wait for the system to fix itself. Patients have power too:- Always ask: “Is this the same as my last prescription?”
- Check the label against the prescription slip.
- Ask: “Why am I taking this? What does it do?”
- Bring a list of all your meds-prescription, over-the-counter, supplements-to every appointment.
- If something looks wrong-wrong color, wrong shape, wrong dose-speak up.
The Future Is Clear: Systems Over Blame
The World Health Organization says medication safety is one of the top five global health priorities. The FDA is pushing for standardized error reporting by 2024. The Pharmacy Quality Alliance wants every pharmacy to use the same classification system by 2025. The message is clear: we need consistency. We need data. We need to stop treating errors as individual failures and start treating them as system failures. The most successful pharmacies aren’t the ones with the most advanced tech. They’re the ones that:- Train staff to speak up without fear
- Build in redundancy for high-risk tasks
- Use technology to support-not replace-human attention
- Learn from every mistake, no matter how small





Write a comment
Your email address will be restricted to us