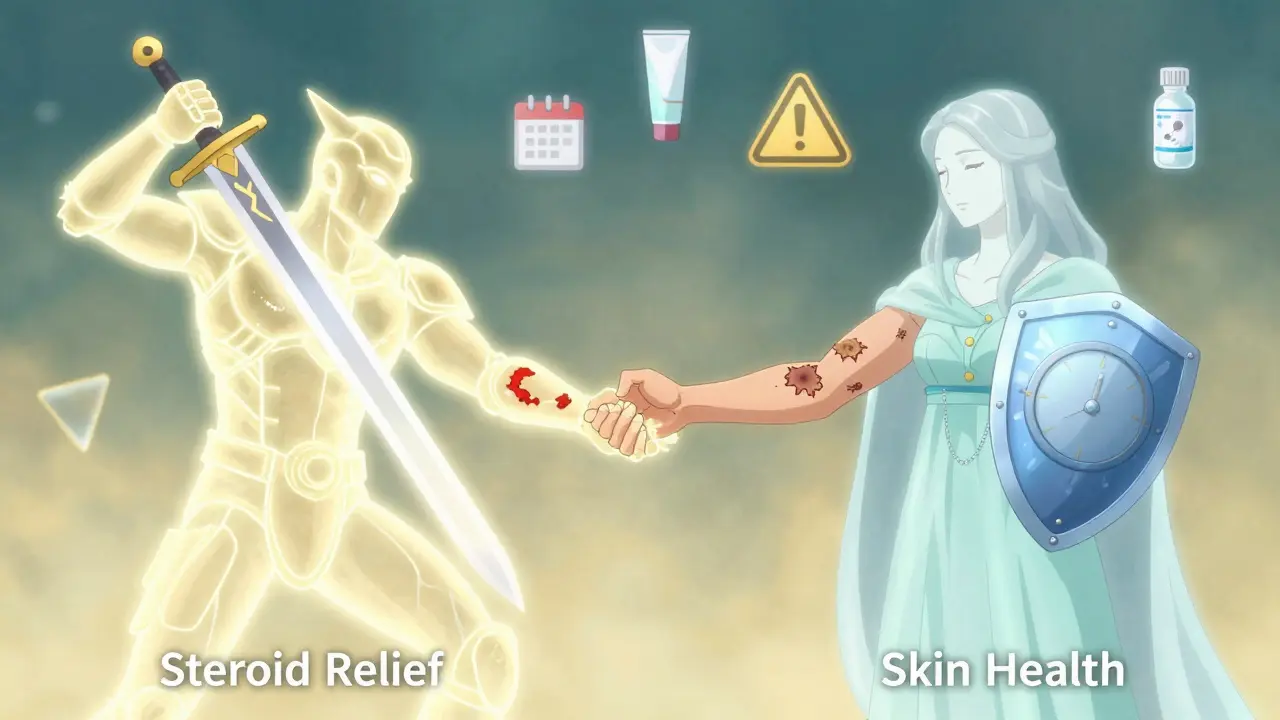
Topical steroids are one of the most common treatments for eczema, psoriasis, and other inflamed skin conditions. They work fast. Many people see improvement in just a few days. But if you use them wrong - too long, too often, or on the wrong parts of your body - you can end up with skin thinning, a real and lasting problem. It’s not rare. It’s not just a myth. It happens. And it’s preventable.
What Are Topical Steroids, Really?
Topical corticosteroids are anti-inflammatory medications you put directly on your skin. They’re not the same as oral steroids you swallow. When applied correctly, they mostly stay on the skin. Skin cells break them down before they enter your bloodstream. That’s why they’re safer than pills for localized problems. But this doesn’t mean they’re harmless. The stronger the steroid, the more powerful the effect - and the greater the risk if misused.
There are seven classes of potency, from mild (Class VII) to super-potent (Class I). Hydrocortisone, the kind you can buy over the counter, is mild. Things like clobetasol or betamethasone? Those are strong. And they’re not meant for daily, long-term use.
How Skin Thinning Happens
Skin thinning, or atrophy, isn’t just about looking fragile. It’s a structural change. The top layer of your skin (the epidermis) and the layer beneath it (the dermis) start to shrink. You might notice:
- Translucent or paper-thin skin
- Visible blood vessels (telangiectasia)
- Easy bruising
- Stretch marks (striae) that don’t fade
- Slower healing after cuts or scrapes
This is most likely to happen on thin skin areas: the face (especially around the eyes and mouth), armpits, groin, and inner thighs. These areas absorb steroids more easily. A 2023 review in StatPearls found that using high-potency steroids on the face for more than two weeks significantly increases the risk of atrophy - and sometimes, it’s permanent.
It’s not just about strength. It’s about duration. Even a mild steroid used daily for months can cause thinning. And it’s not always obvious at first. You might not notice until you see a bruise that won’t go away, or your skin starts tearing when you rub it.
What Doctors Say About Dosing
One of the biggest mistakes patients make? Using too little or too much.
Doctors measure dosage using fingertip units (FTUs). One FTU is the amount of cream or ointment squeezed from a tube onto the last joint of your index finger. It’s not a glob. It’s not a smear. It’s a single line.
Here’s what one FTU covers:
- One hand (front and back): 1 FTU
- One arm (from shoulder to fingertips): 3 FTUs
- One leg: 6 FTUs
- One foot: 2 FTUs
- Entire face and neck: 2.5 FTUs
That’s it. You don’t need to cover every inch in thick layers. A thin, even coat is enough. Rub it in gently until it disappears. More doesn’t mean better. It means more risk.
Application frequency matters too. For strong steroids (Classes I-IV), once a day is all you need. Twice daily offers no extra benefit and increases side effects. That’s according to the American Academy of Family Physicians (2021). For milder versions, twice daily is okay - but only if your doctor says so.

Where Not to Use Strong Steroids
Not all skin is the same. The face, eyelids, groin, and underarms have thinner skin and more blood flow. That means more absorption. That means higher risk.
The GOV.UK guidelines (2023) are clear: only mild steroids (like 1% hydrocortisone) should ever be used on the face. Even then, no longer than five to seven days. Using a potent steroid on your eyelids? That can lead to glaucoma or cataracts. Applying it around your mouth? You might trigger perioral dermatitis - a red, bumpy rash that looks like acne but doesn’t respond to acne treatments.
On the other hand, thick, calloused skin like the palms or soles of the feet can handle stronger formulations. That’s where ointments work best - they’re more occlusive, so they penetrate deeper. But even there, duration matters. No more than two to four weeks without a break.
The Step-Down Strategy
The smartest way to use topical steroids isn’t to use them forever. It’s to use them hard, then back off.
Dr. Jonathan Silverberg, a leading dermatologist, says: “Start strong, then step down.” For example, if you have a bad eczema flare on your arms, you might use a mid-potency steroid twice daily for 10-14 days. Once the redness and itching are gone, switch to a low-potency steroid, then to a non-steroid moisturizer or a calcineurin inhibitor like tacrolimus.
This approach is backed by data. A 2022 study in the Journal of the American Academy of Dermatology found that 85% of dermatologists use this method. Patients who follow it have fewer side effects and longer periods without flares.
It’s not about fear. It’s about control. You’re not stopping treatment - you’re managing it.
What About Non-Steroid Alternatives?
There are other options. Crisaborole, tacrolimus, and pimecrolimus are non-steroidal creams that reduce inflammation without the risk of skin thinning. They’re especially useful for the face and sensitive areas.
But they have downsides. They’re often more expensive. They can cause a burning sensation at first. And they don’t work as fast as steroids. That’s why steroids still dominate - they’re effective, cheap, and fast.
The key is knowing when to use each. Steroids for quick control. Non-steroids for maintenance. And never, ever use steroids long-term as a crutch.
How to Avoid Mistakes
Here’s what works:
- Use the lowest potency that works. Don’t reach for the strongest one just because it “feels better.”
- Apply only once a day for strong steroids. Twice a day for mild ones - if your doctor says so.
- Use fingertip units. Measure it. Don’t guess.
- Never use strong steroids on the face, eyelids, or groin for more than 5-7 days.
- Always combine with a moisturizer - but wait 20-30 minutes between applying steroid and moisturizer. Mixing them reduces effectiveness.
- Stop and call your doctor if you see thinning, bruising, or worsening redness.
- Take breaks. Even if you feel better, don’t keep using it. Let your skin recover.
Many patients think, “I’ll just use it until it’s gone.” But skin conditions like eczema are chronic. They come back. That’s why long-term management matters more than quick fixes.
What Happens When You Stop?
Some people who used strong steroids for months - often without medical advice - report rebound flares when they stop. Their skin gets red, itchy, and burning. This is called topical steroid withdrawal (TSW). It’s not fully understood, but it’s real. It’s more common in people who used high-potency steroids on large areas for over a year.
It’s not an allergic reaction. It’s your skin’s nervous system overreacting after being suppressed for too long. Recovery can take months. Prevention is far easier than treatment.
The UK’s Medicines and Healthcare products Regulatory Agency updated its guidance in June 2023 to warn against unsupervised long-term use. They now require clearer labeling on packaging. But education still lags.
Bottom Line: Steroids Work - If You Use Them Right
Topical steroids are not dangerous. They’re powerful tools. Used with care, they can transform lives. Used carelessly, they can damage skin permanently.
The goal isn’t to avoid them. It’s to use them like a surgeon uses a scalpel - precisely, intentionally, and with full awareness of the risks. Millions of people use them safely every day. The difference? They follow the rules. They know how much to use. They know where not to use it. And they know when to stop.
If you’re using a topical steroid, ask yourself: Am I using it to heal - or to hide? If it’s the latter, it’s time to talk to your doctor.
Can topical steroids cause permanent skin thinning?
Yes, especially with long-term use of high-potency steroids on thin skin areas like the face, armpits, or groin. Skin atrophy can become permanent if the steroids are used for months without breaks. Once the skin loses collagen and elasticity, it doesn’t always return to normal. Early detection and stopping use can prevent lasting damage.
How do I know if I’m using too much steroid?
Signs include skin that looks translucent, easily bruises, shows stretch marks, or feels thin and fragile. If you’re applying more than one fingertip unit per area, or using it more than once daily (for strong steroids), you’re likely overusing it. Also, if you’ve used it continuously for more than two weeks on the face or four weeks elsewhere, you’re at risk.
Is hydrocortisone safe for long-term use?
Even 1% hydrocortisone, the mildest form, shouldn’t be used daily for more than two weeks without medical advice. Long-term use, even of mild steroids, can still cause skin thinning, especially on sensitive areas. It’s not the strength - it’s the duration and frequency that matter.
Why do some doctors prescribe strong steroids for the face?
They shouldn’t - and most don’t. The GOV.UK and American Academy of Dermatology guidelines strictly limit facial use to mild steroids only. If a doctor prescribes a strong steroid for your face, ask why. It might be a mistake, or it might be a short-term plan (e.g., 3-5 days) for a severe flare. Always confirm the plan and duration.
Can I use moisturizer with topical steroids?
Yes - and you should. Moisturizers help repair the skin barrier and reduce flares. But apply the steroid first, wait 20-30 minutes, then apply moisturizer. If you mix them, the steroid won’t work as well. This is a common mistake that reduces effectiveness and prolongs treatment.
Are there alternatives to steroids for eczema?
Yes. Non-steroidal options like crisaborole (Eucrisa) and calcineurin inhibitors (tacrolimus, pimecrolimus) are effective for long-term use, especially on the face and folds. They don’t cause skin thinning. But they’re more expensive and may cause initial burning. They’re best used after steroids have controlled a flare.
What should I do if I think I have skin thinning from steroids?
Stop using the steroid immediately. See a dermatologist. They can confirm if it’s atrophy and recommend a recovery plan. This may include switching to non-steroidal treatments, using emollients daily, and avoiding triggers. Healing can take months. Don’t restart steroids without professional guidance.







Write a comment
Your email address will be restricted to us