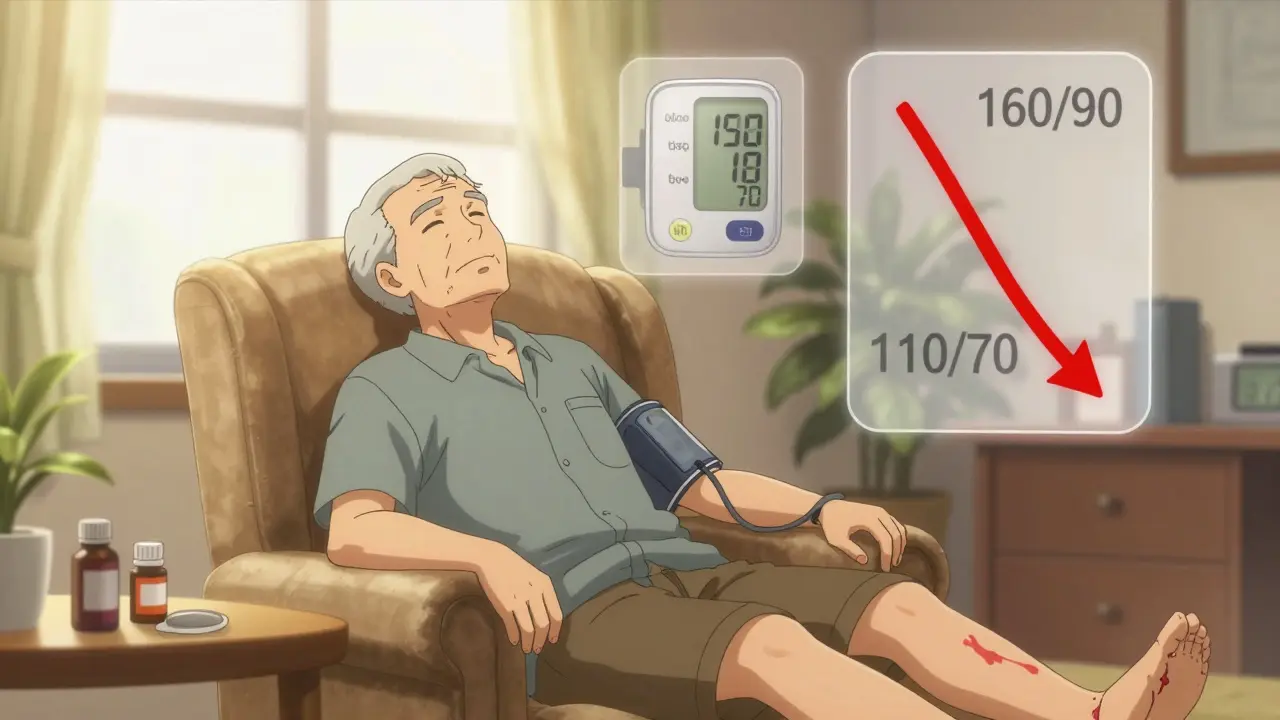
Standing up from a chair and feeling dizzy? That’s not just old age-it could be orthostatic hypotension, a dangerous side effect of blood pressure meds in older adults. It’s more common than you think: up to 26% of seniors on antihypertensives experience a sudden drop in blood pressure when they stand, leading to falls, fractures, and hospital visits. The scary part? Many doctors still think lowering blood pressure too much causes this. But new evidence says the opposite is true.
What Exactly Is Orthostatic Hypotension?
Orthostatic hypotension (OH) isn’t just lightheadedness. It’s a measurable drop in blood pressure-20 mm Hg systolic or 10 mm Hg diastolic-within three minutes of standing. This happens because the body’s natural system for keeping blood flowing to the brain slows down with age. Baroreceptors, those pressure sensors in your neck and chest, don’t respond as quickly. Blood pools in your legs, and your brain gets less oxygen. The result? Dizziness, blurred vision, or even fainting.It’s not rare. In people over 65 with high blood pressure, OH shows up in 3% to 26% of cases, depending on how many meds they’re on and how old they are. And here’s the twist: it’s often not the high blood pressure causing the problem-it’s the medicine meant to treat it.
Which Blood Pressure Meds Are Riskiest?
Not all antihypertensives are created equal when it comes to OH risk. Some are safer than others, and knowing the difference can prevent falls.- Alpha blockers (like doxazosin, terazosin) carry the highest risk-up to 28% of seniors on these meds develop OH. They relax blood vessels too aggressively, especially when standing.
- Beta-blockers (metoprolol, atenolol) double or even triple the odds of sustained low blood pressure when standing. Their effect on heart rate and vessel tone makes them especially risky in older adults.
- Diuretics (furosemide, hydrochlorothiazide) reduce blood volume, which can make standing blood pressure crash. This is worse if you’re not drinking enough water.
- Central sympatholytics (clonidine, methyldopa) suppress the nervous system’s ability to adjust blood pressure on the fly. These are rarely first-line anymore, but still linger in some prescriptions.
On the flip side, two classes are much safer:
- ACE inhibitors (lisinopril, enalapril) and ARBs (losartan, valsartan) have the lowest OH risk-only 8-10% of users experience symptoms. Some studies even show they may protect against OH by improving blood vessel function.
- Calcium channel blockers vary. Amlodipine and lacidipine are well-tolerated because they dilate vessels slowly. But diltiazem and verapamil can cause more OH due to how they’re metabolized in aging livers.
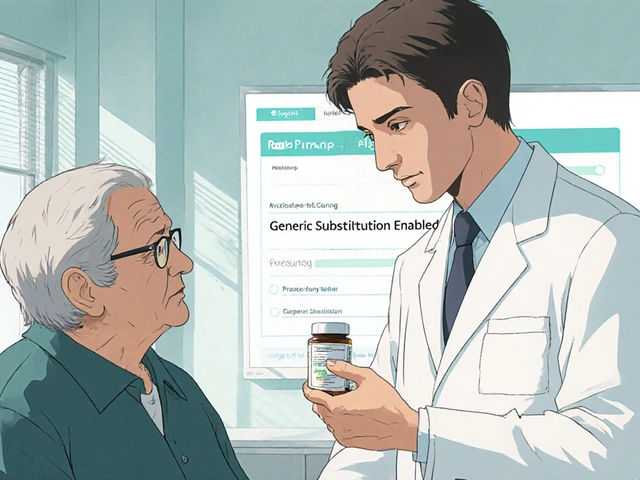
One 2023 analysis found that switching from an alpha blocker to an ARB led to a 65% drop in dizziness and falls among seniors. That’s not luck-it’s science.
More Aggressive Blood Pressure Control? It’s Actually Safer
For decades, doctors were told: "Don’t push blood pressure too low in older adults-you’ll cause orthostatic hypotension." That advice is outdated.The SPRINT trial, which tracked nearly 10,000 adults over 50, showed that targeting a systolic BP under 120 mm Hg (instead of 140) didn’t increase OH. In fact, it slightly lowered it-14.5% in the standard group vs. 14.7% in the intensive group. A separate analysis of 18,500 patients across nine trials found that aggressive treatment actually reduced OH risk by 17%.
Why? Because uncontrolled high blood pressure damages the very systems that regulate standing pressure. When you treat hypertension properly, you’re not just protecting your heart-you’re helping your body adapt better to posture changes.
Dr. Harry Goldblatt, a leading hypertension researcher, put it bluntly: "The real danger isn’t the drop when you stand-it’s the high pressure when you’re lying down." If you stop meds to fix dizziness, you might be trading one risk for a worse one: stroke or heart attack.

What to Do Before Changing Meds
Don’t stop or switch meds on your own. But do ask your doctor these questions:- "Am I on a medication known to cause orthostatic hypotension?"
- "Can we check my blood pressure both lying down and standing?"
- "Is there a safer alternative with the same effect?"
- "Could my dose be lowered without losing control of my BP?"
Many seniors are on multiple meds-some for heart disease, others for depression or prostate issues. A full medication review is critical. The American Geriatrics Society Beers Criteria flags alpha blockers, certain beta-blockers, and tricyclic antidepressants as potentially inappropriate for older adults due to OH risk.
Don’t assume dizziness is just "getting older." It’s a red flag.
Non-Medication Strategies That Work
Even if you stay on the same meds, you can cut OH risk dramatically with simple habits:- Stand up slowly. Sit on the edge of the bed for 30 seconds before standing. Pause again before walking.
- Drink water before rising. Dehydration makes OH worse. Aim for 6-8 glasses a day, unless you have heart failure.
- Wear compression stockings. These help push blood back up from your legs. Not glamorous, but effective.
- Avoid large meals and hot showers. Both cause blood to pool in your gut or skin, lowering BP further.
- Don’t stand still for long. If you’re waiting in line, shift your weight or march in place.
- Sleep with your head slightly elevated. A 10-15 cm pillow can reduce nighttime BP spikes and morning drops.
These aren’t just tips-they’re proven. Studies show that practicing slow position changes multiple times a day leads to noticeable improvement in 2-4 weeks. Your body learns to compensate.
When Medication for OH Itself Might Be Needed
If lifestyle changes aren’t enough and OH is causing falls, doctors may consider adding a drug specifically for OH:- Midodrine (Orvaten): Tightens blood vessels. Takes effect in 30 minutes, lasts 3-4 hours. Best taken in the morning and early afternoon-never after 6 PM, or you’ll lie down with high BP.
- Droxidopa (Northera): Converts to norepinephrine, helping blood vessels respond. Used for neurogenic OH, like in Parkinson’s.
- Fludrocortisone: Helps retain salt and water. Risky for heart failure or kidney disease.
- Pyridostigmine (Mestinon): Improves nerve signaling to blood vessels. Less commonly used, but helpful in some cases.
These aren’t magic pills. They come with side effects and need careful monitoring. But for someone who’s fallen twice in six months, they can be life-changing.
What’s Changing in 2026?
Guidelines are shifting fast. The European Society of Cardiology is finalizing new recommendations for managing hypertension in patients with OH-expected late 2024. The American Geriatrics Society updated its Beers Criteria in 2023 to strengthen warnings against alpha blockers and certain beta-blockers in seniors.Research is moving toward "smart" medications that only dilate blood vessels when you’re lying down-not when you stand. Two compounds are already in Phase II trials. In five years, personalized BP treatment based on posture risk may become standard.
For now, the message is clear: treat high blood pressure aggressively-but choose the right drugs. Avoid the high-risk ones. Use the safer ones. And never ignore dizziness when standing. It’s not normal. It’s a signal.
What to Ask Your Doctor at Your Next Visit
Bring this list to your appointment:- "Is my current blood pressure medication on the list of drugs linked to orthostatic hypotension?"
- "Can we do a standing BP test today?"
- "Would switching to an ARB or ACE inhibitor reduce my risk of dizziness?"
- "Am I on any non-BP meds that could make this worse-like antidepressants or prostate pills?"
- "Should I be wearing compression stockings or adjusting my fluid intake?"
Don’t wait for a fall to happen. A simple conversation now could prevent a hospital stay later.
Is orthostatic hypotension the same as regular dizziness?
No. Regular dizziness can come from inner ear problems, stress, or low blood sugar. Orthostatic hypotension is specifically tied to a drop in blood pressure that happens within three minutes of standing. It’s measurable, predictable, and often linked to medications. If you feel lightheaded only when standing up-especially after lying down or eating-it’s likely OH.
Can I stop my blood pressure meds if I get dizzy?
Never stop without talking to your doctor. Stopping meds to fix dizziness can cause your blood pressure to spike while lying down, increasing your risk of stroke or heart attack. The goal isn’t to lower BP as much as possible-it’s to find the right balance. Your doctor can switch you to a safer drug instead.
Do all seniors on blood pressure meds get orthostatic hypotension?
No. Only 3% to 26% of older adults with hypertension experience it, depending on their meds, age, and other health conditions. People on alpha blockers or multiple diuretics are at highest risk. Those on ACE inhibitors or ARBs have much lower rates. It’s not inevitable-it’s often preventable with the right choices.
How often should blood pressure be checked in older adults on these meds?
When starting or changing a blood pressure medication, check both lying and standing BP within 1-2 weeks. After that, check every 3-6 months-or sooner if you feel dizzy. Home monitoring helps, but standing measurements are essential. Many clinics skip this step, so ask for it.
Are there any foods or supplements that help with orthostatic hypotension?
Yes. Increasing salt intake slightly (if you don’t have heart or kidney disease) can help maintain blood volume. Drinking 16 oz of water before standing can boost BP temporarily. Caffeine in the morning may help too. But avoid alcohol-it worsens OH. Always check with your doctor before making dietary changes, especially if you’re on diuretics.



Write a comment
Your email address will be restricted to us