When your liver is failing, your kidneys don’t just slow down-they can shut down entirely, even if they’re structurally fine. This isn’t a coincidence. It’s hepatorenal syndrome, a deadly chain reaction triggered by advanced liver disease. Unlike typical kidney failure, where damage is visible under a microscope, HRS is a silent collapse of blood flow. The kidneys aren’t broken; they’re starved. And without quick action, survival is measured in days, not months.
What Exactly Is Hepatorenal Syndrome?
Two Types, Two Timelines
Hepatorenal syndrome doesn’t come in one flavor-it has two distinct forms, each with its own pace and prognosis. Type 1 is the emergency. It’s fast, brutal, and often mistaken for a simple infection or dehydration. Within two weeks, serum creatinine doubles to over 2.5 mg/dL. Patients go from barely noticeable fatigue to needing dialysis in under a month. Without treatment, the median survival is just 2 weeks. This isn’t a slow decline-it’s a freefall.
Type 2 is quieter, but no less dangerous. Creatinine creeps up slowly, between 1.5 and 2.5 mg/dL. It’s tied to stubborn ascites-fluid that won’t go away, no matter how much diuretic you give. Patients might feel bloated for months, but the real threat is the slow erosion of kidney function. While Type 1 demands urgent intervention, Type 2 is a ticking clock. It doesn’t kill as fast, but it almost always leads to transplant candidacy-or death.
Why Do Kidneys Fail When the Liver Breaks?
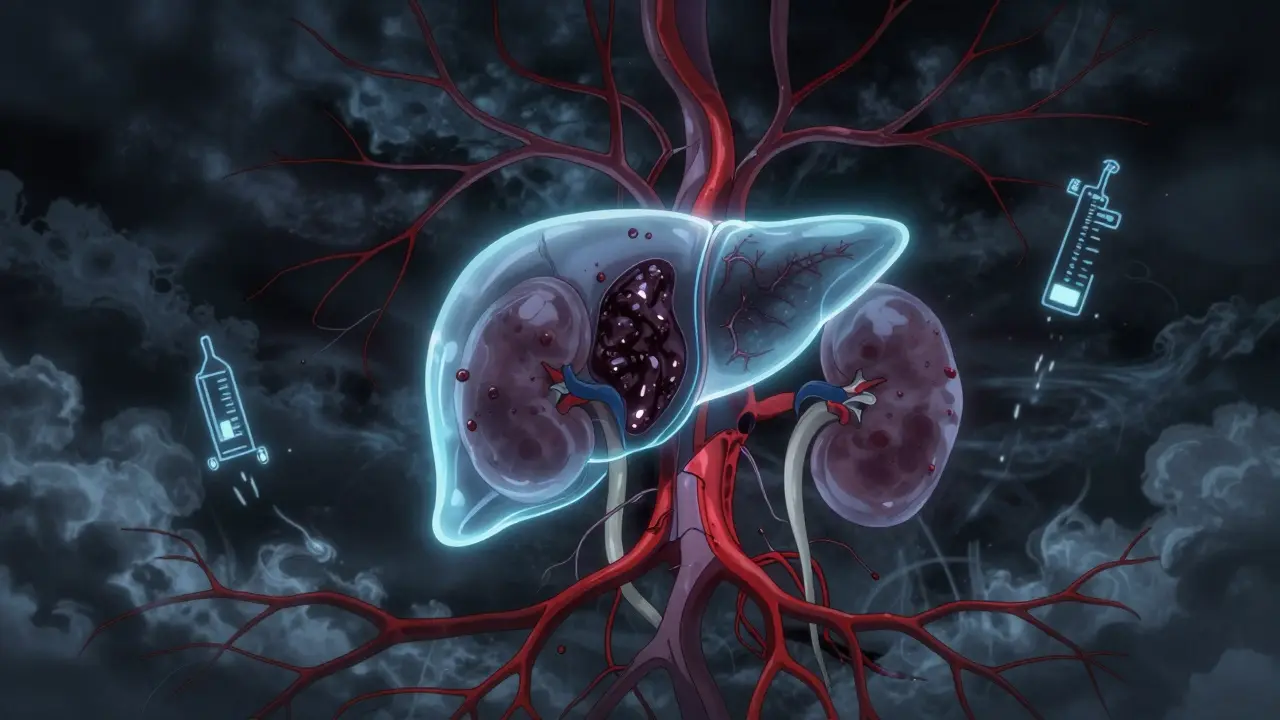
It’s not about the kidneys. It’s about blood pressure. In cirrhosis, scar tissue blocks blood flow through the liver. That forces blood to find other routes, flooding the gut area with too much pressure. The vessels there widen-too much, too fast. This drops overall blood pressure in the body’s main arteries. The body panics. It thinks it’s drowning in fluid, even though it’s not. So it tightens every blood vessel it can, especially in the kidneys. That’s the problem. The kidneys get less blood. Less filtration. Less urine. Creatinine climbs. But if you take a biopsy? No scarring. No damage. Just silence.
This isn’t theory. Studies show renal blood flow drops by 40-50% in HRS. Glomerular filtration rate-how well kidneys clean blood-plummets by 60-70%. The body’s stress systems-RAAS, sympathetic nerves, antidiuretic hormone-all go into overdrive, trying to save the situation. But they’re fighting the wrong battle. The kidneys aren’t the enemy. The liver is.

What Triggers the Collapse?
Most HRS cases don’t come out of nowhere. Something pushes the liver over the edge. The biggest trigger? Spontaneous bacterial peritonitis-SBP. In 35% of cases, a simple infection in the belly fluid sets off the cascade. Other common triggers: upper GI bleeding (22%), severe alcohol flare-ups (11%), and even overuse of diuretics or NSAIDs. These aren’t minor events. They’re red flags. If you have cirrhosis and suddenly stop making urine, or your belly swells more than ever, don’t wait. Get tested.
Doctors must rule out everything else first. No protein in urine? No blood? No blockage? No recent kidney toxin exposure? Then it’s likely HRS. The key test: after pulling diuretics and giving 1 gram per kg of albumin (up to 100g), does kidney function improve within 48 hours? If not, HRS is the diagnosis. Too many patients are misdiagnosed because this step is skipped. One study found 25-30% of HRS cases are missed or confused with other kidney injuries.
How Is It Treated?
There’s no magic pill. But there’s a proven path. The first step is always stopping anything that hurts the kidneys-NSAIDs, antibiotics like aminoglycosides, even too much salt. Then comes albumin. Lots of it. 1g per kg on day one, then 20-40g daily. This helps restore blood volume and gives the kidneys a fighting chance.
For Type 1, the gold standard is terlipressin. It’s a vasoconstrictor that tightens the over-dilated blood vessels in the gut, redirecting blood back to the kidneys. Given every 4-6 hours, it can bring creatinine down in 10-14 days. In clinical trials, 44% of patients responded. One patient shared online: “My creatinine was 3.8. After 10 days of terlipressin, it dropped to 1.9. But the stomach cramps were awful.” That’s common. Side effects include heart rhythm issues, low blood pressure, and even tissue death in fingers or toes from too much vasoconstriction.
In the U.S., terlipressin (brand name Terlivaz™) was approved by the FDA in December 2022. It costs about $1,100 per vial. A full 14-day course? Around $13,200. Many insurers still fight coverage. Some hospitals still use the older combo of midodrine and octreotide-less effective, but cheaper. One Reddit user wrote: “My husband didn’t respond to midodrine for six weeks. We’re now on the transplant list with a MELD-Na of 28.”
Transplant: The Only Real Cure
Medication can buy time. But only a liver transplant fixes the root problem. Survival without transplant? For Type 1, only 18% live a year with supportive care. With terlipressin and albumin? 39%. But with a transplant? 71%. That’s the difference between a chance and a cure.
That’s why experts now recommend listing for transplant as soon as Type 1 HRS is diagnosed-even if creatinine drops with treatment. The 2023 ELITA guidelines say: don’t wait for improvement. If you have HRS, you need a new liver. The MELD-Na score, which ranks transplant priority, now includes kidney function. That means HRS patients jump ahead in line. A 15-20% boost in priority can mean the difference between life and death.
What’s on the Horizon?
Research is moving fast. New biomarkers like NGAL (neutrophil gelatinase-associated lipocalin) in urine might detect HRS before creatinine even rises. The PROGRESS-HRS trial is testing whether a cutoff of 0.8 ng/mL can predict HRS before it happens. If it works, doctors could intervene before kidney failure starts.
Other drugs are in trials: alfapump® for managing ascites in Type 2, and PB1046, a new vasopressin agonist. But access remains a huge problem. In North America, 63% of HRS patients get vasoconstrictors. In sub-Saharan Africa, that number is 11%. Most get only fluids and diuretics-nothing that targets the real cause.
What Should You Do If You or a Loved One Has Cirrhosis?
If you have advanced liver disease, know the signs: less urine, sudden swelling, confusion, dizziness. Don’t assume it’s just fluid retention. Ask your doctor: “Could this be hepatorenal syndrome?” Demand the albumin challenge test. Push for a liver specialist if your doctor isn’t familiar with HRS. Most community hospitals don’t have protocols. Only 35% of U.S. hospitals do. But academic centers? Nearly all have hepatology consult teams.
Track your creatinine. Know your MELD-Na score. If it’s above 25, you’re in high-risk territory. Get on the transplant list early. HRS isn’t a side effect-it’s a warning. And warnings, when ignored, become obituaries.
Is hepatorenal syndrome the same as acute kidney injury?
No. Acute kidney injury (AKI) is a broad term for any sudden drop in kidney function. Hepatorenal syndrome is a specific type of AKI that happens only in people with advanced liver disease, and it’s caused by blood flow problems-not direct kidney damage. Other causes of AKI include dehydration, infection, or toxins. HRS is diagnosed only after those are ruled out.
Can hepatorenal syndrome be reversed without a transplant?
Yes, sometimes. In Type 1 HRS, terlipressin and albumin can restore kidney function in about 44% of patients. In Type 2, treatments like TIPS (a shunt procedure) can improve kidney function in 60-70% of cases. But these are temporary fixes. Without a liver transplant, HRS almost always returns. The underlying liver disease hasn’t been cured.
Why is terlipressin not widely available in the U.S.?
Terlipressin was not FDA-approved until December 2022. Before that, doctors used off-label alternatives like midodrine and octreotide, which are less effective. Even now, many hospitals and insurers are slow to adopt it due to cost-about $13,200 for a two-week course. Access is better in transplant centers but still limited in community hospitals.
What’s the difference between Type 1 and Type 2 hepatorenal syndrome?
Type 1 is rapid and life-threatening-creatinine doubles to over 2.5 mg/dL in under two weeks. Type 2 is slower, with creatinine between 1.5 and 2.5 mg/dL, and it’s tied to fluid buildup (ascites) that doesn’t respond to diuretics. Type 1 needs urgent treatment; Type 2 is a longer-term problem that often leads to transplant listing.
Can hepatorenal syndrome be prevented?
You can reduce your risk. Avoid alcohol completely. Take antibiotics if you have spontaneous bacterial peritonitis. Don’t use NSAIDs like ibuprofen. Stay hydrated, but don’t overdo diuretics. Get regular blood tests to track creatinine and sodium. And if you have cirrhosis, get on the transplant list early-before your kidneys start failing.
Final Thoughts: Time Is the Enemy
Hepatorenal syndrome doesn’t care how young you are or how healthy you were before. It doesn’t care if you’ve been told your liver is ‘stable.’ It only cares about one thing: whether you’ve been recognized in time. The window for treatment is narrow. The stakes are high. If you’re living with cirrhosis, don’t wait for symptoms to get worse. Know your numbers. Ask the right questions. Push for a specialist. Because in HRS, survival isn’t about luck-it’s about action.





Write a comment
Your email address will be restricted to us