Gut Health Risk Assessment Calculator
Gut Health Assessment
Your gut health significantly impacts allergic responses. This tool helps you evaluate how your daily fiber intake supports a healthy gut microbiome and may reduce allergy risk.
Your Gut Health Assessment
Enter your daily fiber intake above to see how it affects your gut health and allergy risk.
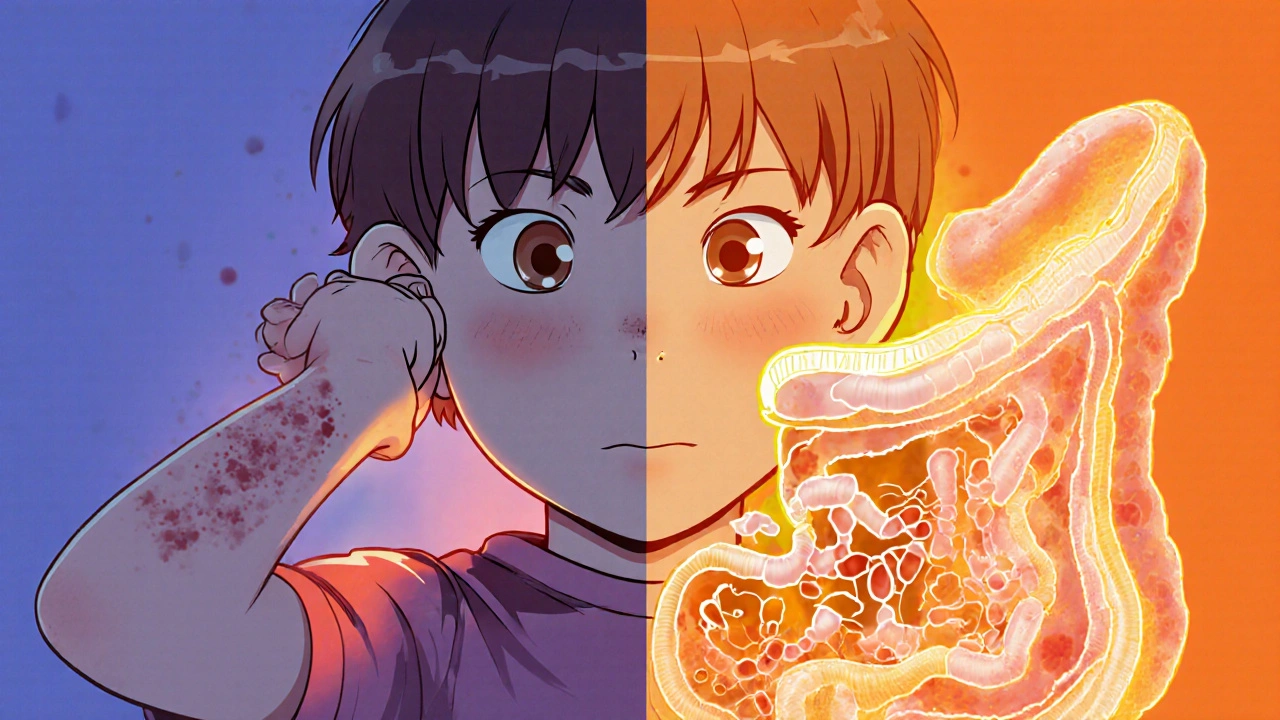
Ever wonder why some people seem to develop allergies out of nowhere while others never do? The answer often starts deep inside, where trillions of microbes call home. Gut health plays a surprisingly powerful role in shaping the body’s allergic responses.
Key Takeaways
- Gut microbiota communicate with the immune system, influencing allergy development.
- Imbalances such as reduced diversity or "leaky gut" can increase risk for food allergies, eczema, asthma, and more.
- Targeted diet changes, probiotics, and prebiotics can restore balance and lessen symptoms.
- Early‑life microbial exposure is critical; breastfeeding and diverse foods matter.
- Professional guidance is essential for severe or persistent allergic conditions.
Understanding Gut Health
Gut Health is a state of the gastrointestinal tract where the lining, digestion, and resident microbes function harmoniously. When the gut operates smoothly, it filters out toxins, extracts nutrients, and trains the immune system to recognize friend from foe. But when the balance tips-say, after antibiotics or a low‑fiber diet-the gut’s protective shield weakens.
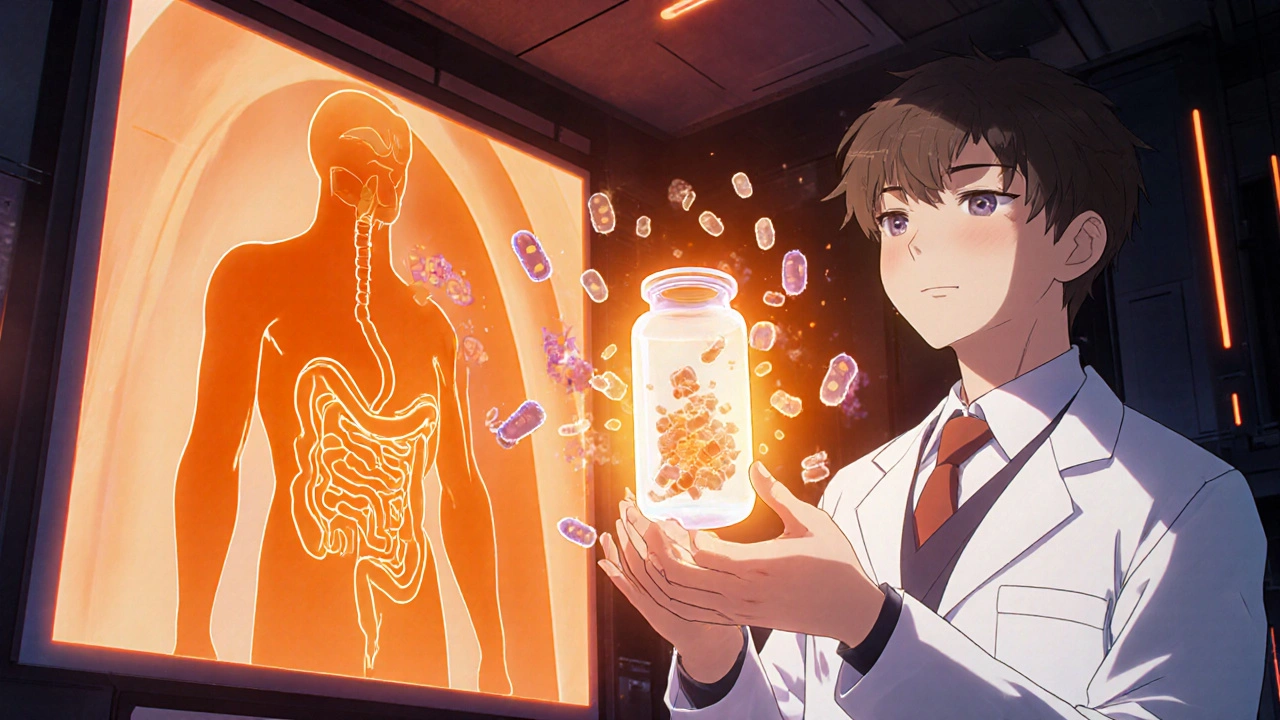
How the Gut Connects to the Immune System
The gut houses about 70% of the body’s immune cells, making it an immunological command center. The wall‑lining cells, called Enterocytes, constantly sample microbial metabolites and inform immune cells whether to calm down or gear up.
One key messenger is Short‑chain fatty acids (SCFAs) such as acetate, propionate, and butyrate. Produced when bacteria break down fiber, SCFAs act as anti‑inflammatory agents, encouraging regulatory T‑cells that keep allergic reactions in check.
What Are Allergic Disorders?
Allergic Disorders are conditions where the immune system overreacts to harmless substances, releasing histamine and other chemicals that cause symptoms ranging from itching to breathing difficulty. Common types include food allergy, atopic dermatitis (eczema), allergic rhinitis, and asthma.
While genetics set the stage, gut‑derived signals determine whether the script ends with tolerance or hypersensitivity.
Key Gut‑Related Factors Behind Allergies
Research points to several gut mechanisms that tip the balance toward allergy:
- Dysbiosis: Reduced microbial diversity, especially lower levels of Bifidobacterium and Lactobacillus, correlates with higher allergy rates.
- Leaky Gut: When tight junctions loosen, larger food particles slip into the bloodstream, prompting an IgE‑mediated response.
- Low SCFA Production: A fiber‑poor diet cuts SCFA output, weakening regulatory T‑cell development.
- Histamine‑producing Bacteria: Certain strains (e.g., Clostridia) release histamine directly, amplifying allergy symptoms.
Evidence from Recent Studies
A 2024 meta‑analysis of 38 cohort studies found that infants fed a high‑fiber, probiotic‑rich diet had a 30% lower odds of developing eczema by age two. Another 2025 randomized trial showed that a 12‑week course of Probiotics containing Lactobacillus rhamnosus GG reduced the severity of allergic rhinitis scores by 22% compared to placebo.
Animal models also reveal a causal link: germ‑free mice (lacking gut microbes) develop exaggerated airway inflammation when exposed to dust mites, a response that normalizes after fecal microbiota transplantation from healthy donors.
Practical Steps to Support Gut Health for Allergy Prevention
Below is a quick‑reference table summarizing actionable gut factors and how they influence allergic outcomes.
| Gut Factor | Impact on Allergies | Example Food / Supplement |
|---|---|---|
| Fiber‑rich diet (SCFA boost) | Strengthens regulatory T‑cells → lower IgE | Whole grains, legumes, berries |
| Probiotic intake | Increases beneficial Bifidobacterium/Lactobacillus | Yogurt with live cultures, kefir |
| Prebiotic supplementation | Feeds good bacteria, improves barrier function | Inulin, chicory root, garlic |
| Avoid excess processed sugars | Reduces growth of histamine‑producing microbes | Swap soda for water |
| Omega‑3 fatty acids | Anti‑inflammatory, supports gut lining | Fatty fish, flaxseed oil |
Implement these habits gradually. Start with one change-like adding a daily serving of fermented vegetables-and track any reduction in allergy flare‑ups.
Special Considerations for Different Age Groups
Infants and toddlers: Breast milk supplies natural prebiotics (human milk oligosaccharides) that nurture Bifidobacterium. Introducing a variety of solid foods after six months, while avoiding unnecessary antibiotics, sets a strong microbial foundation.
Children and adolescents: School lunches often lack fiber. Encourage snacks like apple slices with almond butter or homemade trail mix with pumpkin seeds to keep gut microbes thriving.
Adults: Stress and alcohol can disrupt gut motility. Mind‑body practices (yoga, meditation) and limiting alcohol to two drinks per week help maintain barrier integrity.
When to Seek Professional Help
If you notice persistent hives, wheezing, or gastrointestinal distress after eating certain foods, consult an allergist or gastroenterologist. They may recommend:
- Allergy testing (skin prick or serum IgE) to pinpoint triggers.
- Stool analysis to assess microbial diversity.
- Targeted probiotic formulations based on lab results.
- Elimination diets supervised by a dietitian.
Self‑treating severe reactions can be dangerous; professional guidance ensures safety and effectiveness.
Future Directions: Microbiome‑Based Therapies
Scientists are exploring next‑generation treatments such as personalized fecal transplants and engineered bacterial strains that produce anti‑allergic compounds on demand. While still in trials, these approaches hint at a future where we can "rewire" the gut to prevent or even cure certain allergies.
Can taking a probiotic cure my food allergy?
Probiotics can reduce the severity of some food allergies, especially in children, but they rarely eliminate the allergy entirely. They work best when combined with other strategies like dietary adjustments and medical supervision.
What foods are highest in prebiotic fiber?
Top sources include chicory root, Jerusalem artichoke, garlic, onions, leeks, asparagus, and bananas. Adding a serving of any of these each day boosts the beneficial bacteria that protect against allergies.
Is "leaky gut" a real medical condition?
The term describes increased intestinal permeability, which can be measured by specific lab tests. While not all doctors use the phrase, the underlying physiology-tight‑junction disruption-is well documented.
How early should I start focusing on my baby's gut health?
From birth! Breastfeeding, avoiding unnecessary antibiotics, and introducing a range of age‑appropriate solid foods after six months lay a strong foundation.
Are there risks to using high‑dose probiotics?
In healthy individuals, high doses are usually safe, but people with compromised immune systems or severe gut disorders should consult a doctor first, as rare infections have been reported.



Write a comment
Your email address will be restricted to us