Pregnancy Medication Safety Checker
Rosuvastatin & Pregnancy Safety Assessment
This tool helps you understand when to safely stop rosuvastatin before conception and what alternatives are available for cholesterol management during pregnancy.
Your Safety Assessment
Results will appear here after clicking the button above.
Expecting a baby brings a flood of questions, especially when you’re already on medication for high cholesterol. One drug that often pops up is rosuvastatin. Is it safe? Should you stop it? This guide walks you through the science, the official recommendations, and practical steps you can take, so you can make an informed decision without the guesswork.
Key Takeaways
- Rosuvastatin is classified as a Category X medication by the FDA, meaning it’s generally advised against during pregnancy.
- Major health agencies (FDA, NICE, AHA) recommend stopping rosuvastatin before conception and using non‑statin options if cholesterol control is still needed.
- Evidence from human and animal studies shows an increased risk of fetal malformations at high doses, but data are limited for typical therapeutic levels.
- If you discover you’re pregnant while on rosuvastatin, consult your provider immediately to discuss a safe transition plan.
- Lifestyle changes, bile‑acid sequestrants, and omega‑3 supplements are the most common alternatives during pregnancy.
What Is Rosuvastatin?
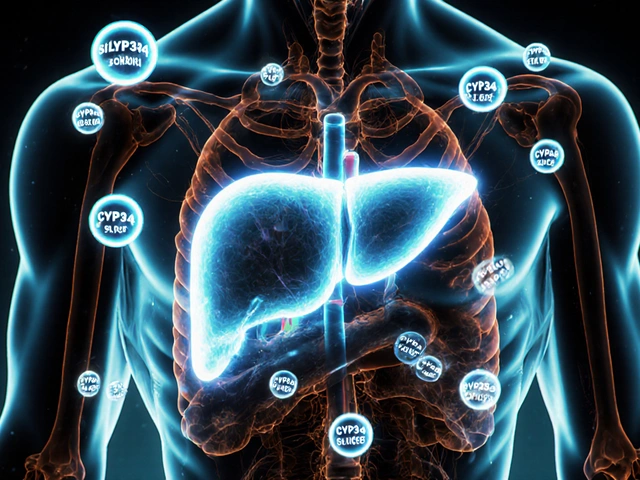
Rosuvastatin is a synthetic statin medication that lowers low‑density lipoprotein (LDL) cholesterol by inhibiting the HMG‑CoA reductase enzyme in the liver. It was approved by the U.S. Food and Drug Administration (FDA) in 2003 and quickly became popular because of its potency and once‑daily dosing.
How Statins Work & Cholesterol Basics
Statins, including rosuvastatin, belong to a broader class of drugs that target the cholesterol‑synthesis pathway. By blocking HMG‑CoA reductase, they reduce the production of LDL cholesterol, the "bad" cholesterol linked to heart attacks and strokes.
While lowering LDL is crucial for cardiovascular health, the pregnancy period introduces unique considerations. Cholesterol is a building block for fetal cell membranes and hormones, so the maternal body naturally adjusts lipid metabolism during the second and third trimesters.
Pregnancy & Medication Safety Overview
Pregnancy is a physiological state that alters how drugs are absorbed, distributed, metabolized, and excreted. Because the developing fetus is especially vulnerable, regulatory agencies assign pregnancy risk categories to medications.
The FDA uses a lettering system (A, B, C, D, X) to indicate potential harm. Category X means “contraindicated in pregnancy” - the risks clearly outweigh any possible benefits. NICE (National Institute for Health and Care Excellence) follows a similar precautionary stance, advising clinicians to avoid statins in women who are pregnant or planning a pregnancy.
Official Guidelines on Rosuvastatin Use in Pregnancy
Both the FDA and international bodies such as NICE and the American Heart Association (AHA) converge on a cautious approach:
- Stop rosuvastatin at least three months before attempting conception.
- If pregnancy is discovered while on the drug, discontinue immediately unless a specialist justifies continued use.
- Re‑evaluate cardiovascular risk after delivery; many women can safely restart therapy postpartum.
| Statin | FDA Pregnancy Category | Evidence Level | Recommended Use in Pregnancy |
|---|---|---|---|
| Rosuvastatin | X | Animal studies show teratogenic effects; limited human data | Avoid - discontinue before conception |
| Atorvastatin | X | Similar animal data; case reports of birth defects | Avoid - same as rosuvastatin |
| Pravastatin | X | Animal teratogenicity, some small human cohort studies | Avoid - not recommended |
| Simvastatin | X | Animal data strong; human data scarce | Avoid - standard practice |
Risks and Findings from Recent Studies
Research up to 2024 paints a consistent picture:
- A 2021 multinational cohort (over 12,000 pregnancies) found a 1.8‑fold increase in major congenital malformations among women who filled a statin prescription in the first trimester.
- Animal studies (rat and rabbit) show dose‑dependent skeletal and craniofacial abnormalities when exposed to rosuvastatin.
- Some observational data suggest that low‑dose rosuvastatin after the first trimester may not significantly raise risk, but the evidence remains weak and clinicians err on the side of caution.
Because the data are not robust enough to declare rosuvastatin “safe,” the default recommendation stays at Category X.
What to Do If You’re Already on Rosuvastatin and Discover You’re Pregnant
- Contact your healthcare provider immediately. Do not stop the medication on your own unless advised.
- Expect a thorough review of your cardiovascular risk profile. Your doctor may order a lipid panel to see how your numbers have changed since stopping.
- If you have a high risk of heart disease (e.g., prior heart attack, severe hyperlipidemia), a specialist might consider a short‑term alternative, but this is rare.
- Switch to pregnancy‑compatible options when needed. The most common choices are:
- Bile‑acid sequestrants (e.g., cholestyramine) - they bind cholesterol in the gut and are not absorbed.
- Omega‑3 fatty acids (e.g., EPA/DHA supplements) - generally regarded as safe and can modestly improve triglyceride levels.
- Intensive lifestyle changes - diet low in saturated fat, regular moderate exercise, and weight management.
- Plan for postpartum re‑evaluation. Most women can restart rosuvastatin or another statin 6‑12 weeks after delivery, once breastfeeding status is clarified.
Alternatives for Managing Lipids During Pregnancy
While statins sit on the “avoid” shelf, many other strategies keep cholesterol in check without harming the baby:
- Dietary tweaks: Focus on high‑fiber foods, plant sterols (found in fortified spreads), and omega‑3 rich fish like salmon (cooked, not raw).
- Physical activity: Aim for at least 150 minutes of moderate‑intensity aerobic exercise per week, unless contraindicated.
- Non‑statin medications: Bile‑acid sequestrants are the go‑to pharmacologic choice; they have been used safely in pregnancy for decades.
- Monitoring: Regular lipid panels each trimester help track any concerning rise, allowing early diet or medication adjustments.
Frequently Asked Questions
Can I take rosuvastatin during the second or third trimester?
Current guidelines still advise against any trimester. The lack of solid human data means clinicians prefer to avoid potential risks altogether.
What if I stopped rosuvastatin before getting pregnant but my cholesterol is now high?
Start with lifestyle changes first. If LDL remains above target, discuss bile‑acid sequestrants with your doctor. Post‑delivery, you can usually resume rosuvastatin.
Are there any statins considered safer than rosuvastatin in pregnancy?
All statins share the same FDA Category X rating. None are officially deemed safe for use during pregnancy.
Will stopping rosuvastatin affect my baby’s development?
Stopping the drug reduces any theoretical risk of drug‑induced birth defects. The fetus still gets enough cholesterol from the mother’s natural production.
How long should I wait after stopping rosuvastatin before trying to conceive?
Most experts recommend a wash‑out period of at least three months, which covers the drug’s half‑life and ensures steady‑state clearance.
Bottom line: when it comes to rosuvastatin and rosuvastatin pregnancy concerns, err on the side of caution. Talk to your cardiologist or obstetrician, explore safe alternatives, and keep your heart health in check without compromising your baby’s safety.


Write a comment
Your email address will be restricted to us