Ever wondered why a medication that stops seizures might also dim your mood? topiramate depression link isn’t a myth-it’s a real concern that doctors and patients wrestle with every day. In this article we break down what topiramate does, why it can trigger depressive symptoms, who’s most vulnerable, and how to stay on top of your mental health while taking the drug.
What Is Topiramate?
Topiramate is an anticonvulsant medication approved by the FDA for epilepsy and migraine prevention. First marketed in 1996, it quickly became popular because it also promotes weight loss, a side effect that many patients find appealing.
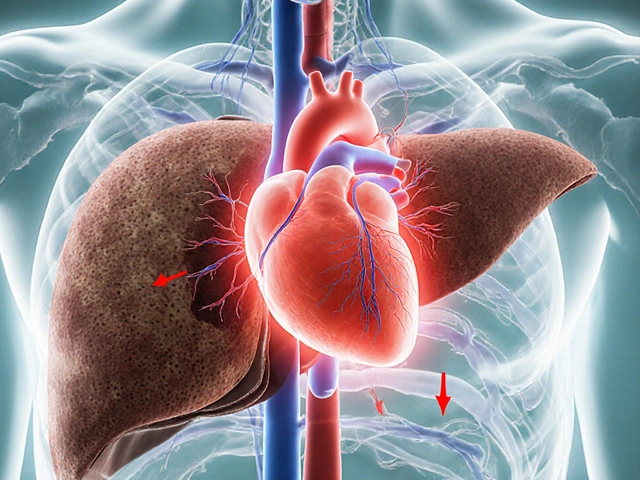
How Does Topiramate Work?
Topiramate’s exact mechanism is still a puzzle, but researchers agree it modulates several brain pathways:
- GABA enhancement: Boosts the brain’s main inhibitory neurotransmitter, calming neuronal firing.
- Glutamate inhibition: Blocks excitatory NMDA receptors, reducing seizure activity.
- Carbonic anhydrase inhibition: Alters pH balance, which can affect neuronal excitability.
- Sodium channel blockade: Dampens rapid firing of nerve cells.
These actions explain why topiramate controls seizures and migraines, but they also touch on the chemical systems that regulate mood.
Common Side Effects (Beyond Seizures)
Most patients tolerate topiramate well, yet a predictable set of side effects shows up in clinical trials:
- Peripheral tingling (paresthesia)
- Word‑finding difficulty (cognitive slowing)
- Weight loss (up to 10 % of body weight)
- Kidney stones (rare)
- Dry mouth and taste alteration
Notice that many of these involve the brain’s communication pathways-precisely the same pathways that influence mood.
Depression: A Quick Primer
Depression is a mood disorder characterized by persistent sadness, loss of interest, and a range of physical symptoms such as fatigue and changes in appetite. The World Health Organization estimates that over 264 million people worldwide experience depression each year.
While genetics, stress, and chronic illness dominate the conversation, medications can either protect against or provoke depressive episodes.
Scientific Evidence Linking Topiramate to Depression
Several studies have explored the relationship:
- Randomized controlled trials (RCTs) for migraine: In a 2012 meta‑analysis of 12 RCTs (≈1,800 participants), the pooled risk ratio for new‑onset depression was 1.48 (95 % CI 1.12-1.95) compared with placebo.
- Epilepsy cohorts: A 2018 retrospective review of 2,340 epilepsy patients found that 8.3 % developed depressive symptoms after starting topiramate, versus 4.7 % on other anticonvulsants.
- Weight‑loss trials: Because rapid weight loss can itself trigger mood swings, a 2020 trial that combined topiramate with lifestyle counseling reported a higher incidence of depressive episodes (12 % vs 5 % in control).
These numbers aren’t catastrophic, but they signal a clear pattern-particularly at higher doses (≥200 mg/day) and in people with a personal or family history of mood disorders.
Who Is Most at Risk?
Risk isn’t uniform. The following factors increase the odds of topiramate‑related depression:
- Pre‑existing mood disorder: Patients with prior major depressive disorder or bipolar disorder are the most vulnerable.
- High dosage: Doses above 200 mg per day markedly raise the risk.
- Rapid weight loss: Losing more than 5 % of body weight in the first month can destabilize mood.
- Concurrent serotonergic drugs: Interaction with SSRIs or SNRIs may amplify emotional blunting.
- Age and gender: Young adults (18‑30) and women report mood changes more frequently.
Monitoring and Managing Depression While on Topiramate
Early detection saves both mental health and the effectiveness of the original treatment. Here’s a practical approach:
- Baseline assessment: Before starting topiramate, document mood using the PHQ‑9 questionnaire.
- Scheduled check‑ins: Re‑assess at 2‑week, 1‑month, and 3‑month intervals. Ask specific questions: "Have you felt unusually sad or hopeless?"
- Dosage tweaking: If depressive symptoms emerge, try reducing the dose by 25 % and observe for 2 weeks.
- Adjunct therapy: Adding a low‑dose SSRI (e.g., sertraline 25 mg) can counteract mood dips without compromising seizure control.
- Switching agents: When symptoms persist despite adjustments, discuss alternatives such as levetiracetam for epilepsy or propranolol for migraine prophylaxis.
Never stop topiramate abruptly; withdrawal can trigger seizures or rebound headaches.
Alternatives When Depression Becomes a Deal‑Breaker
Not every patient needs to abandon topiramate. However, for those whose quality of life suffers, consider these options:
| Condition | Alternative Drug | Key Benefits | Typical Dose |
|---|---|---|---|
| Epilepsy (partial seizures) | Levetiracetam | Low cognitive side‑effects, minimal mood impact | 500‑1500 mg/day |
| Migraine prophylaxis | Propranolol | Well‑studied, no depressive signal | 40‑240 mg/day |
| Weight loss (off‑label) | Phentermine‑topiramate (Qsymia) - lower topiramate component | Combines appetite suppression with modest weight loss | 7.5 mg topiramate component |
Switching should be done under specialist supervision, especially for seizure control.
Quick Checklist for Patients on Topiramate
- Know your baseline PHQ‑9 score.
- Track mood daily for the first 2 months.
- Report any loss of interest, hopelessness, or thoughts of self‑harm immediately.
- Maintain regular follow‑up appointments.
- Discuss dosage changes before making them yourself.
- Consider a mental‑health professional if symptoms persist beyond 2 weeks.
Bottom Line
Topiramate is a powerful tool for seizure control and migraine prevention, but it carries a measurable risk of depressive symptoms-especially at higher doses and in mood‑vulnerable individuals. By establishing a baseline, monitoring regularly, and being ready to adjust dosage or switch drugs, patients can enjoy the benefits without sacrificing mental well‑being.
Can topiramate cause severe depression?
Severe depression is rare, but the risk rises with higher doses and pre‑existing mood disorders. If you notice intense sadness, loss of interest, or suicidal thoughts, seek medical help right away.
Do antidepressants interact with topiramate?
Most SSRIs and SNRIs are safe, but they can blunt the mood‑lifting effect of topiramate’s weight loss. Your doctor may start at a low antidepressant dose and watch for side‑effects.
How long does it take for depression symptoms to appear after starting topiramate?
Symptoms often emerge within the first 4‑6 weeks, aligning with the period of rapid weight loss and dose escalation.
Is it safe to stop topiramate if I feel depressed?
Abrupt cessation can trigger seizures or rebound migraines. Always taper under a physician’s guidance and discuss alternative treatments.
Are there lifestyle steps that reduce the depression risk?
Maintain steady weight loss (no more than 1-2 % per week), stay physically active, get adequate sleep, and practice stress‑relief techniques like mindfulness.





Write a comment
Your email address will be restricted to us