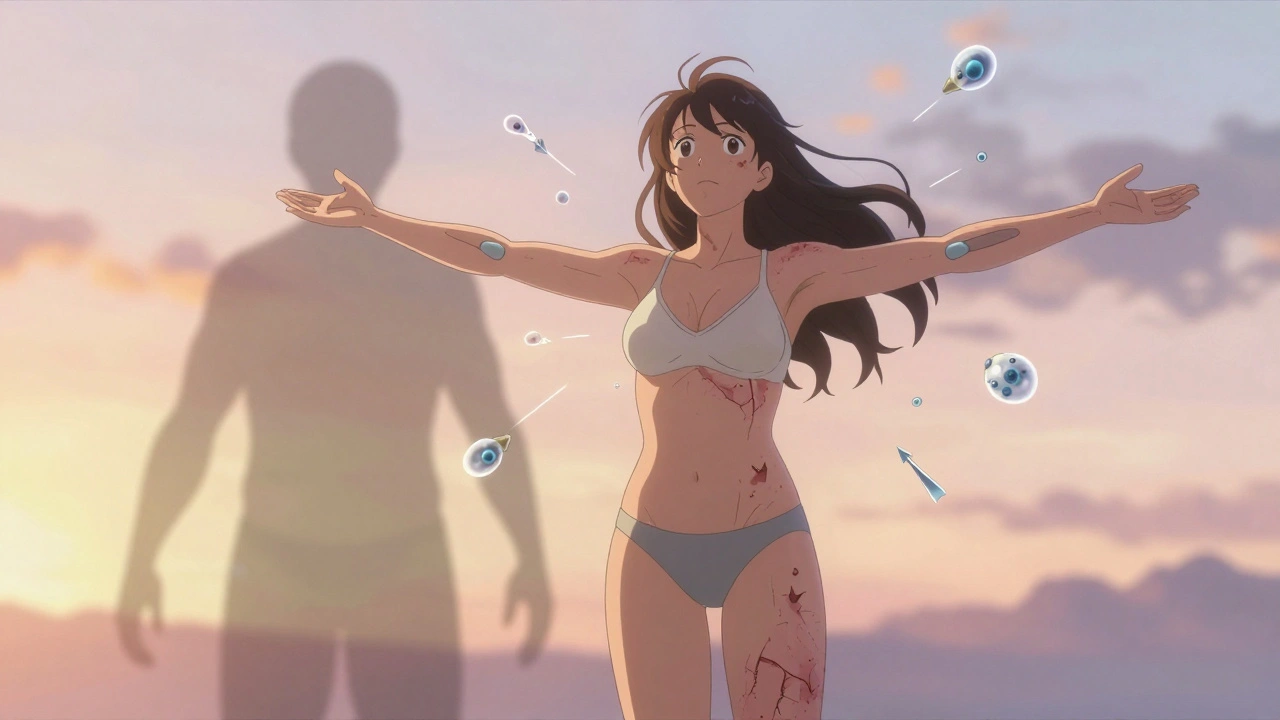
When your skin breaks out in red, scaly patches, it’s easy to think it’s just a cosmetic issue. But for nearly one in three people with psoriasis, that skin flare-up is a warning sign - something deeper is going on. Their immune system isn’t just attacking their skin. It’s also turning on their joints, tendons, and even their nails. This isn’t just a skin condition. It’s psoriatic arthritis - a full-body autoimmune disease that can change your life if left unchecked.
What Exactly Is Psoriatic Arthritis?
Psoriatic arthritis (PsA) doesn’t appear out of nowhere. It usually shows up in people who already have psoriasis - a chronic skin condition marked by thick, silvery scales and inflamed red patches. About 30% of people with psoriasis will eventually develop PsA, according to the American College of Rheumatology’s 2022 guidelines. In most cases, the skin comes first: 85% of people notice psoriasis years before their joints start hurting. But in 5-10% of cases, joint pain shows up before any skin changes. That’s why doctors now look at the whole picture - not just the rash. PsA isn’t just arthritis. It’s a mix of problems: swollen fingers that look like sausages (called dactylitis), inflamed tendons where they attach to bone (enthesitis), pitted or crumbling nails, and pain in the lower back or neck. These aren’t random symptoms. They’re all signs your immune system is on a rampage, attacking healthy tissue in multiple places at once.How Is It Diagnosed?
There’s no single blood test for PsA. Diagnosis relies on putting together clues. Doctors use the CASPAR criteria - a set of rules developed in 2006 that’s now the gold standard. To confirm PsA, you need inflammatory joint disease plus at least three of these:- Current or past psoriasis (3 points)
- Psoriatic nail changes like pitting or lifting (1 point)
- Negative rheumatoid factor (1 point)
- Typical bone changes on X-ray (1 point)
- Family history of psoriasis (2 points)
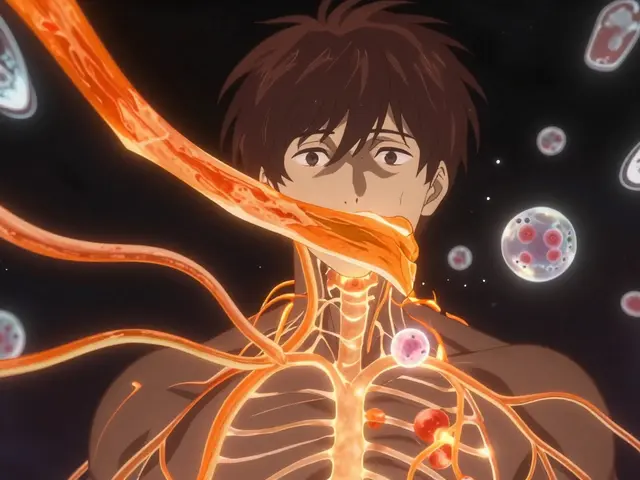
What Happens Inside Your Body?
Your immune system normally protects you from germs. In PsA, it gets confused. It starts attacking your own cells - especially in the skin, joints, and entheses (the spots where tendons and ligaments connect to bone). Scientists have found strong links to certain genes, especially HLA-B27, HLA-B38, and HLA-B39. If you have a family member with psoriasis or PsA, your risk goes up. But genes alone don’t cause it. Something triggers it - stress, infection, injury, or even gut changes. Recent research shows PsA patients have different gut bacteria than healthy people. That’s why scientists are now studying the “gut-skin-joint axis” - how your digestive system might be fueling inflammation in your skin and joints. The real damage comes from overactive immune signals. Tumor necrosis factor-alpha (TNF-α), interleukin-17 (IL-17), and interleukin-23 (IL-23) are key players. These proteins act like alarm bells, telling your body to keep attacking. That’s why drugs that block them work so well.
What Are the Symptoms?
PsA doesn’t look the same in everyone. Here’s what to watch for:- Joint pain and swelling: Fingers, toes, knees, wrists, and lower back are common. Often asymmetric - one side of the body is worse than the other.
- Dactylitis: Entire fingers or toes swell up like sausages. Happens in about 40% of cases.
- Enthesitis: Pain where tendons attach to bone - especially the Achilles tendon or bottom of the foot. Affects 35-50% of patients.
- Nail changes: Pitting, ridges, thickening, or nails lifting off the nail bed. Seen in 80% of PsA patients.
- Skin plaques: Red, scaly patches, often on elbows, knees, scalp, or lower back. Present in 80-90% of cases.
- Back and neck pain: If your spine is involved, you might feel stiffness in the morning that improves with movement.
- Fatigue: Not just tiredness - a deep, bone-weary exhaustion that doesn’t go away with rest.
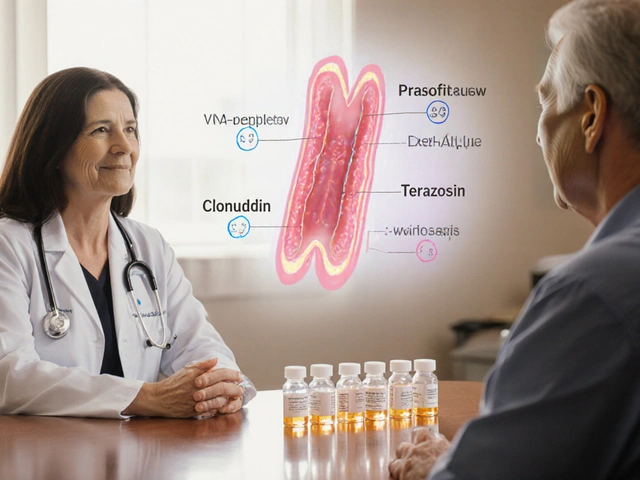
Treatment: Stopping the Damage Before It’s Too Late
The goal isn’t just to reduce pain. It’s to reach minimal disease activity - a specific target that keeps damage from worsening. That means:- Tender joints ≤1
- Swollen joints ≤1
- Psoriasis covers ≤1% of your skin
- Pain score ≤15 on a 100-point scale
- Quality of life score ≤0.5 on the HAQ scale
- TNF inhibitors: Adalimumab, etanercept, infliximab. Great for joint and spine pain. About 50-60% of patients see a 20% improvement (ACR20).
- IL-17 inhibitors: Secukinumab, ixekizumab. Better for skin psoriasis. Often clear skin completely.
- IL-23 inhibitors: Guselkumab, risankizumab. Newer, very effective for skin and joints.
- JAK inhibitors: Tofacitinib. Taken as a pill, not an injection. Works when other drugs fail.
Comorbidities: The Hidden Dangers
PsA isn’t just about joints and skin. It’s a systemic disease. People with PsA have a 43% higher risk of heart attack. About half have metabolic syndrome - high blood pressure, belly fat, high blood sugar, and bad cholesterol. Depression and anxiety affect 20-30% of patients. Quality of life scores are 30-40% lower than in people without PsA. Mortality is 30-50% higher than average - mostly because of heart disease. That’s why treatment isn’t just about the rash or the ache. It’s about protecting your whole body. Doctors now screen for high blood pressure, diabetes, and depression as part of routine care.What’s Next? The Future of PsA Care
Research is moving fast. New drugs like deucravacitinib (a TYK2 inhibitor) and bimekizumab (which blocks both IL-17A and IL-17F) are showing great results in trials. By 2027, experts predict 70% of PsA patients will be on biologics or targeted drugs within two years of diagnosis - up from 40% today. Blood tests for biomarkers like calprotectin and MMP-3 might soon help predict who’ll respond to which drug. High-resolution MRI and ultrasound are catching inflammation before it causes permanent damage. And the gut connection? It’s no longer just theory. Early studies suggest probiotics and dietary changes might help calm inflammation. More trials are underway.What Should You Do If You Suspect PsA?
If you have psoriasis and notice joint pain, stiffness, or swollen fingers - don’t wait. See a rheumatologist. If you have joint pain without a rash, but a family history of psoriasis - get checked. Early treatment can stop joint damage before it starts. You don’t have to live with constant pain. You don’t have to accept fatigue as normal. PsA is serious - but it’s treatable. With the right care, most people can reach minimal disease activity and live full, active lives.Can psoriasis turn into psoriatic arthritis?
Yes. About 30% of people with psoriasis develop psoriatic arthritis. In most cases, skin symptoms appear years before joint pain - but in 5-10% of cases, joint problems come first. Not everyone with psoriasis gets PsA, but if you notice swelling, stiffness, or pain in your joints, it’s important to get evaluated.
Is psoriatic arthritis the same as rheumatoid arthritis?
No. While both cause joint inflammation, they’re different diseases. Rheumatoid arthritis usually affects joints symmetrically and is linked to rheumatoid factor in the blood. Psoriatic arthritis often affects joints unevenly, causes dactylitis and enthesitis, and is associated with psoriasis and negative rheumatoid factor. The treatments overlap, but the underlying causes are different.
Can psoriatic arthritis be cured?
There’s no cure yet. But with modern treatments, many people can reach minimal disease activity - meaning little to no pain, no joint damage progression, and clear skin. Early treatment is the key to preventing long-term damage.
What triggers psoriatic arthritis flares?
Common triggers include stress, infections (like strep throat), skin injuries (cuts or sunburns), smoking, heavy alcohol use, and certain medications like lithium or beta-blockers. Gut health and weight gain may also play a role. Identifying your personal triggers can help you manage flares better.
Does psoriatic arthritis affect life expectancy?
Yes, studies show people with PsA have a 30-50% higher risk of early death, mostly due to heart disease and other cardiovascular problems. That’s why managing inflammation isn’t just about joints - it’s about protecting your heart, liver, and overall health. Regular check-ups and controlling risk factors like blood pressure and cholesterol are critical.



Write a comment
Your email address will be restricted to us