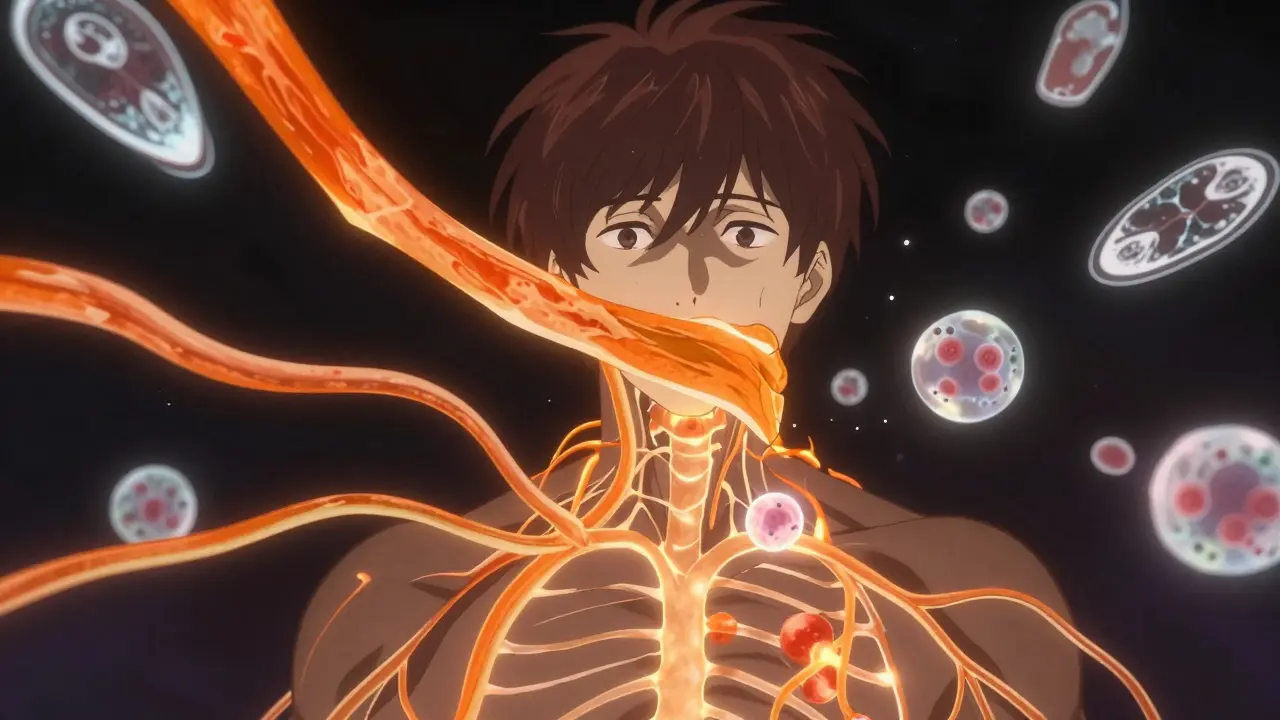
Multiple sclerosis isn’t just one disease-it’s a complex breakdown in how your nervous system talks to the rest of your body. Imagine your nerves as electrical wires, and myelin as the rubber coating around them. In multiple sclerosis, your immune system turns against that coating, stripping it away piece by piece. Without myelin, signals slow down, get lost, or stop completely. That’s when you start feeling numbness, fatigue, trouble walking, or even words slipping out of reach.
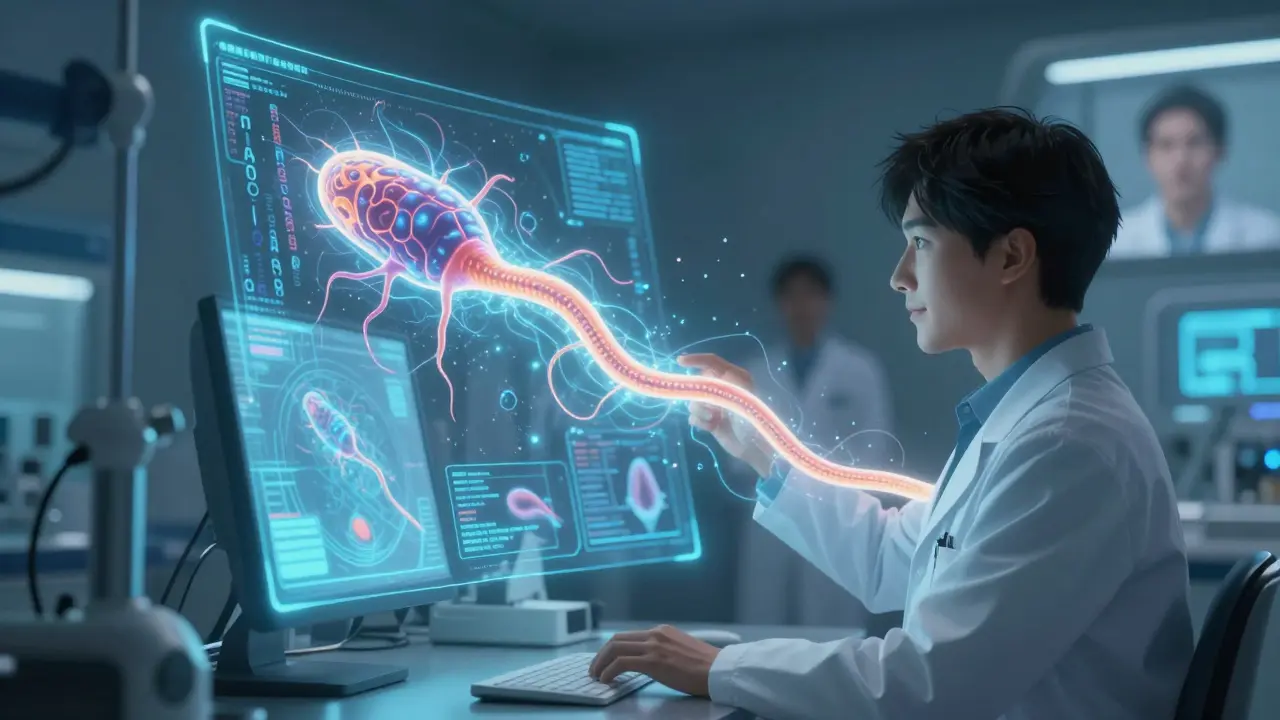
What Actually Happens in Your Body?
Your central nervous system-your brain and spinal cord-is covered in a fatty substance called myelin. It’s made by cells called oligodendrocytes, and its job is simple: speed up nerve signals. Healthy myelin lets impulses race at up to 120 meters per second. In someone with MS, that speed drops by 30 to 50% in damaged areas. The immune system, usually your body’s defense force, starts attacking myelin like it’s a foreign invader. T-cells breach the blood-brain barrier, trigger inflammation, and leave behind hardened scars called plaques. These show up clearly on MRI scans as bright spots, especially when contrast dye is used.
It’s not random. Over 230 genetic variants are linked to higher MS risk, with one gene-HLA-DRB1*15:01-tripling your chance of developing it. But genes alone don’t cause MS. Environmental factors play a huge role. People living farther from the equator are more likely to get it. Canada, Scotland, and Scandinavia have rates as high as 300 per 100,000. Near the equator? Around 30 per 100,000. One big clue? Vitamin D. Low levels-below 30 ng/mL-are tied to a 40% higher risk. Sunlight exposure matters. Places with less than 300 hours of sunshine a year see far more cases than sunnier regions.
Who Gets MS and When?
Most people are diagnosed between ages 20 and 40. Women are two to three times more likely to be diagnosed than men. That gender gap has stayed steady for decades, though researchers still don’t fully understand why. It’s not just age and gender-it’s also geography, lifestyle, and even viruses. A 2022 Harvard study found that people who had infectious mononucleosis (caused by Epstein-Barr virus) were 32 times more likely to develop MS later. But other studies suggest this link might be influenced by other factors like vitamin D or genetics. The truth? It’s a mix.
There’s no single test for MS. Diagnosis takes time-often 6 to 12 months. Doctors use the McDonald Criteria, updated in 2017, which requires proof of damage in at least two different areas of the central nervous system and evidence that those damages happened at different times. MRI scans are the gold standard. A 3 Tesla scanner catches 30% more lesions than older 1.5 Tesla machines. A spinal tap, blood tests, and evoked potential tests (which measure how fast nerves respond to stimuli) help rule out other conditions like Lyme disease or lupus.
The Four Types of MS
Not everyone’s MS looks the same. There are four main patterns, and they change how the disease progresses.
- Clinically Isolated Syndrome (CIS): This is a first episode of neurological symptoms lasting at least 24 hours. If your MRI shows MS-like lesions, you have a 60-80% chance of developing full MS within 10 years.
- Relapsing-Remitting MS (RRMS): This is the most common type-85% of initial diagnoses. People have clear flare-ups (relapses) followed by periods of recovery (remission). Without treatment, they might have 0.5 to 1 relapse per year.
- Secondary Progressive MS (SPMS): After 10 to 25 years, about half to 90% of RRMS patients shift into this phase. Relapses become less frequent, but disability slowly builds. Walking, balance, and bladder control often worsen over time.
- Primary Progressive MS (PPMS): Affects 15% of people from the start. No relapses. Just steady decline. Progression is measured on the Expanded Disability Status Scale (EDSS), with most losing about 1 to 1.5 points per year.
These types aren’t just labels-they shape treatment. RRMS responds best to immune-modifying drugs. PPMS has fewer options, but newer therapies like ocrelizumab have shown real benefits.

What Does MS Feel Like?
Outside of medical reports, real people describe MS in ways numbers can’t capture. On the National MS Society’s MyMSTeam platform, 78% of 150,000 users say fatigue is their worst symptom-not just being tired, but a deep, bone-crushing exhaustion that doesn’t go away with sleep. One Reddit user, u/MSWarrior2020, described trying to speak and having words just disappear: “I know what I want to say, but my brain won’t let me say it.” That’s brain fog, a common and often misunderstood symptom.
Other daily struggles include muscle stiffness, blurred vision, bladder control issues, and tingling in hands or feet. Some people lose balance and fall. Others can’t feel their feet. These aren’t minor inconveniences-they change jobs, relationships, and independence. A 2022 survey found that 82% of working people with MS need accommodations. Flexible hours? 65% asked for it. Remote work? 58%. Without these, many lose their jobs.
Treatment: Slowing the Damage
There’s no cure yet-but there are more tools than ever. Disease-modifying therapies (DMTs) don’t fix damaged nerves, but they slow the immune system’s attacks. There are six main types, from injectables to infusions to pills.
Older drugs like interferon beta-1a help reduce relapses but come with side effects: flu-like symptoms (68% of users), and injection site reactions (76%). That’s why 42% of people stop taking them within a year. Newer drugs like ocrelizumab and ofatumumab are more effective. In one study, 68% of patients on ocrelizumab had no relapses over two years-compared to 45% on older treatments. Ublituximab (Briumvi), approved by the FDA in March 2023, cut relapse rates by 50% compared to teriflunomide.
Cost is a barrier. Annual prices range from $65,000 for generic glatiramer acetate to $87,000 for newer drugs. But 90% of U.S. patients get help through manufacturer copay programs. In countries without strong healthcare systems, access is uneven. The Multiple Sclerosis International Federation reports that 50% of low- and middle-income nations have no access to DMTs at all.
Rehabilitation and Daily Life
Medicines don’t fix everything. Physical therapy is critical. A 2021 Cochrane Review found that balance training reduced falls by 47% in MS patients. Occupational therapy helps with fine motor skills. Speech therapy tackles word-finding problems. Most people need 2-3 sessions a week for 8-12 weeks. Copays under Medicare Part B average $35 per session.
Research is pushing forward. Scientists are testing stem cell therapies-127 active trials as of early 2024. Fecal microbiota transplants (FMT) are being studied for their anti-inflammatory effects, with early results showing a 30% drop in inflammatory markers. One promising drug, ANV419, targets estrogen receptors and cut new brain lesions by 40% in Phase II trials.
The biggest hope? Remyelination. If we can regrow myelin, we might reverse damage. Opicinumab, an experimental drug, improved visual signal speed by 15% in trials. It’s not a cure, but it’s a step toward healing, not just slowing.
What’s Changed in the Last Decade?
Prognosis has improved dramatically. In the 1990s, only 45% of people with MS could walk without help after 20 years. Today, thanks to early diagnosis and better drugs, 70% of those diagnosed after 2010 still walk independently two decades later. That’s not luck-it’s science.
And the future? More precise. Blood tests for neurofilament light chain-a protein released when nerves are damaged-are now used in 37% of clinical trials to track progression faster than MRI. We’re moving from treating symptoms to predicting who will respond to which drug.
One theory that didn’t hold up? The “liberation procedure,” which claimed MS was caused by blocked neck veins. Ten randomized trials with over 1,200 patients found no benefit. It was debunked in 2022. That’s science working as it should-testing, failing, correcting.
What You Need to Know Right Now
MS isn’t a death sentence. Life expectancy is near normal for most people. The goal isn’t to eliminate the disease-it’s to keep it from stealing your life. Early treatment matters. If you’ve had a single neurological episode-numbness, vision loss, weakness-get an MRI. Don’t wait. The sooner you start, the more you protect your nervous system.
Support matters too. Whether it’s online communities like MyMSTeam or local MS societies, connection reduces isolation. You’re not alone. And you’re not powerless. With the right care, many people with MS live full, active lives-working, parenting, traveling, even competing in sports.
The science is moving fast. What’s true today might be outdated in two years. Stay informed. Ask questions. And remember: your experience matters as much as the data.
Is multiple sclerosis hereditary?
MS isn’t directly inherited like eye color, but genetics play a role. If a parent has MS, your risk goes up from about 1 in 750 to 1 in 40. Over 230 gene variants are linked to higher risk, especially HLA-DRB1*15:01. But even with those genes, most people never develop MS. Environment and lifestyle matter just as much.
Can stress cause multiple sclerosis?
Stress doesn’t cause MS, but it can trigger flare-ups. Studies show that major life events-like losing a job or a death in the family-can increase relapse risk in the weeks that follow. Managing stress through sleep, exercise, or therapy doesn’t stop MS, but it helps keep symptoms under control.
Does diet affect multiple sclerosis?
No single diet cures MS, but what you eat can influence inflammation and energy levels. Diets rich in omega-3s, vegetables, and fiber-like the Mediterranean diet-are linked to better outcomes. Avoiding processed foods and excess sugar helps manage fatigue. Vitamin D is especially important; low levels are tied to higher disease activity.
Can you get MS after age 50?
Yes, though it’s less common. About 10% of MS diagnoses happen after 50. Late-onset MS often looks more like primary progressive MS, with steady decline instead of clear relapses. Diagnosis can be harder because symptoms are sometimes mistaken for normal aging or other conditions like stroke or Parkinson’s.
Are there natural treatments for MS?
Supplements like vitamin D, omega-3s, and probiotics may help manage symptoms and reduce inflammation, but they don’t replace disease-modifying drugs. Practices like yoga, acupuncture, and mindfulness can improve quality of life and reduce stress. But no herbal remedy or supplement has been proven to stop MS progression. Always talk to your neurologist before starting anything new.
Will I need a wheelchair?
Not necessarily. In the 1990s, about 55% of people with MS needed a wheelchair after 20 years. Today, thanks to early treatment, only about 30% do. Many people use canes, walkers, or mobility scooters for energy conservation-not because they can’t walk, but to preserve stamina. Staying active, doing physical therapy, and starting treatment early are the best ways to keep mobility.
Can women with MS have children?
Yes. Pregnancy doesn’t worsen MS long-term. In fact, relapse rates drop by up to 70% during the third trimester. The risk of relapse increases in the first 3-6 months after birth, but overall, most women with MS have healthy pregnancies and babies. Many DMTs are safe to stop before conception and restart after breastfeeding. Talk to your neurologist and OB-GYN early to plan.
What Comes Next?
If you’ve just been diagnosed, give yourself time to process. MS isn’t a single event-it’s a journey. The first step is finding a neurologist who specializes in MS. The second is starting treatment as soon as possible. The third? Building your support system. Whether it’s family, online groups, or local chapters, you don’t have to do this alone.
If you’re living with MS and feeling stuck, remember: progress isn’t always linear. Some days are hard. Others are bright. What matters is that you’re still here, still fighting. And the science? It’s still moving forward. Every year, more people get better tools. More treatments. More hope.




Write a comment
Your email address will be restricted to us